The Centers for Medicare & Medicaid Services (CMS) released the Medicare Physician Fee Schedule (PFS) Final Rule on Oct. 30, 2015. It addresses changes to the PFS as well as other important Medicare Part B payment policies. The rule became effective Jan. 1, 2016, and was published in the Nov. 16, 2014, Federal Register.
Explore This Issue
ACEP Now: Vol 35 – No 01 – January 2016Conversion Factor
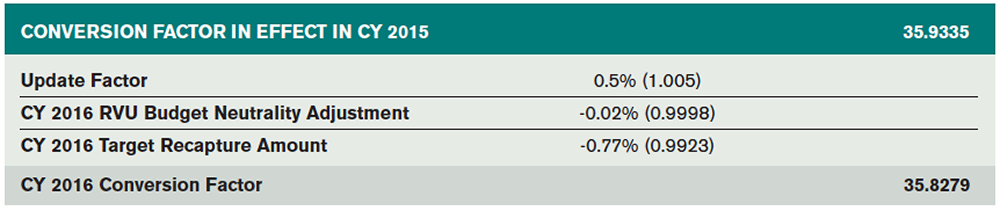
At the conclusion of 2015, the Medicare conversion factor (the amount Medicare pays per Relative Value Unit [RVU]) was set at $35.9335. The 2016 rule is no longer governed by the Sustainable Growth Rate (SGR) formula, which had mandated continuing annual cuts to physician payments, resulting in year-after-year Congressional rescues with short-term fixes. Instead, with the passage of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), signed into law on April 16, 2015, the draconian SGR cuts were permanently repealed and the conversion factor was stabilized. In addition to broad sweeping payment reform related to Physician Quality Reporting System (PQRS), the value-based payment modifier (VBM), meaningful use, and alternative payment models, MACRA provides positive annual payment updates of 0.5 percent through 2019. However, due to two additional pieces of legislation—Protecting Access to Medicare Act of 2014 (PAMA) and Achieve a Better Life Experience Act of 2014, which mandate net cost savings of 1 percent—the final 2016 conversion factor will actually be decreased by 0.3 percent. As a result, the 2016 Final Rule published a conversion factor of $35.8279 (see Table 1).
Merit-Based Incentive Program
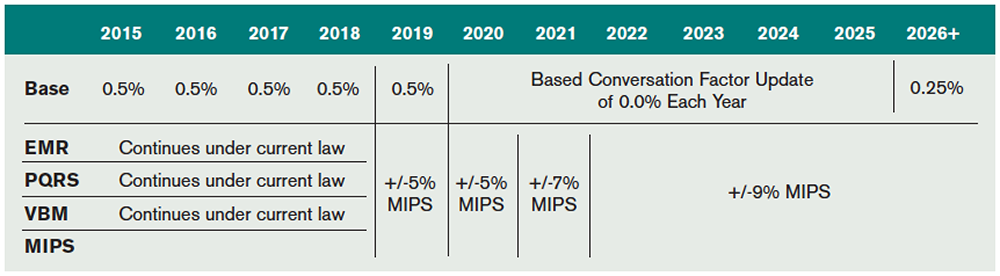
The Merit-Based Incentive Payment System (MIPS) is a new payment mechanism that will provide annual updates to physicians starting in 2019 based on performance in four categories: quality, resource use, clinical practice improvement activities, and meaningful use of an electronic medical record (EMR) system.
Unlike the flawed SGR, the new system will adjust payments based on individual performance. Importantly, MIPS does not set an arbitrary aggregate spending target, which previously led to the need for annual patches to prevent SGR-mandated cuts. The three existing quality programs (PQRS, VBM, and EMR) will be consolidated under MIPS beginning in 2019. An overview of the evolution of the various federal quality programs is in Table 2.
Geographic Practice Cost Index Update
The Geographic Practice Cost Index (GPCI) is used by CMS to modify the RVU values based on regional differences relating to cost of living, malpractice, and practice cost/expense, which allows Medicare to adjust reimbursement rates taking into account regional and practice-specific factors. Some states have a permanently fixed work GPCI, including Alaska at 1.5 and the frontier states (Montana, Nevada, North Dakota, South Dakota, and Wyoming) at 1.0. Other states are subject to a work RVU GPCI that ranges from 0.6 to 1.2. In past years, Congress passed single-year legislation, setting a GPCI work floor of 1.0 that then expired at the end of the year. Section 102 of PAMA allowed for another extension of the work GPCI floor, and the existing 1.0 floor on the physician work GPCI was extended through March 31, 2016.
ED E/M RVUs Stable for 2016
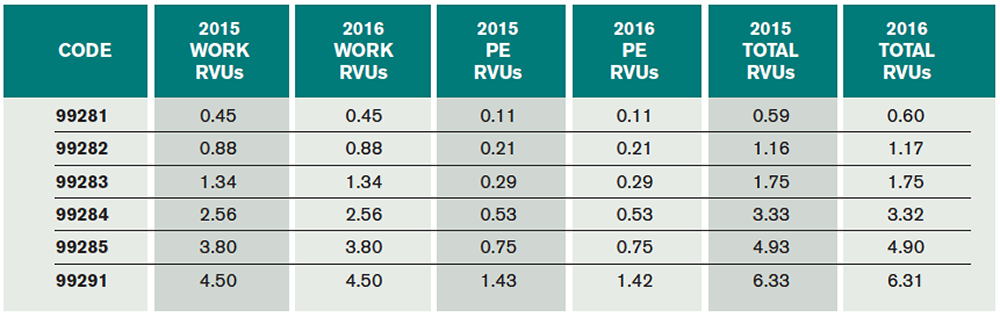
Emergency medicine’s RVU values are stable for 2016, with only small decimal point–level changes. For 2016, the work RVUs for emergency medicine services remain unchanged. The total RVUs (work, malpractice, and practice expense RVUs) associated with ED E/M services 99281–99285 and 99291 will experience small changes driven by adjustments in practice expense and liability expense. The CMS-published specialty-specific impact analysis states that emergency medicine will experience a 0 percent update in overall RVU values for 2016. The 0 percent increase for emergency medicine as a specialty published by CMS contains moderate rounding. Though accurate for 99283, the RVUs for many of the other ED codes are minimally decreased at the hundredth of an RVU level (see Table 3).
Critical Care Services
Critical care services were also revalued as part of the Final Rule and benefited from a small increase (see Table 4).
Physician Quality Reporting System
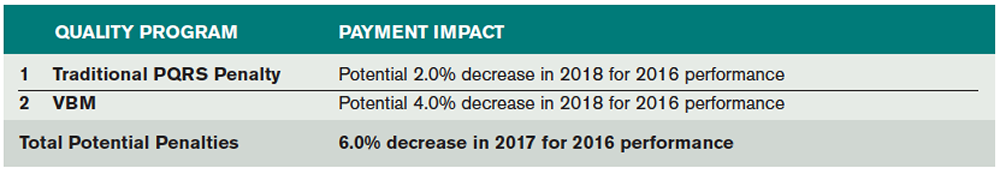
PQRS continues for 2016. Groups not reporting PQRS measures in 2016 will receive a 2 percent penalty assessed against their 2018 Medicare allowables. Additionally, failing to satisfy 2016 PQRS reporting requirements would trigger an additional 4 percent penalty for most groups under the VBM program for a total penalty of 6 percent in 2018.
For 2016, satisfactory PQRS reporting requires at least nine measures, involving three National Quality Strategy domains, for at least 50 percent of the Medicare part B patients during the year. Additionally, the 2015 requirement for reporting on a cross-cutting measure continues for 2016.
The predominant 2016 potential CMS ED PQRS measures typically applicable to ED providers are listed in Table 5. There are also three new measures related to head CT utilization, including head CT for adult blunt head trauma, head CT use in the pediatric population, and use of neuroimaging in patients with a primary headache.
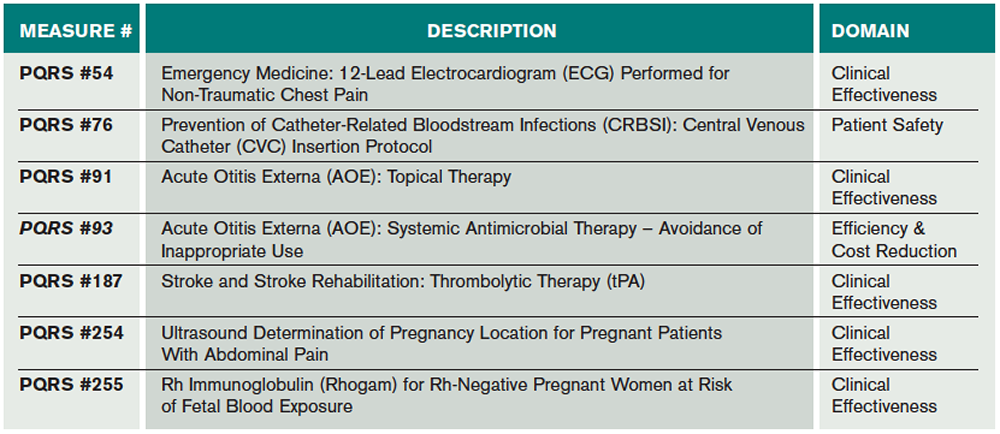
(click for larger image) Table 5. Predominant 2016 Potential CMS ED PQRS Measures Typically Applicable to ED Providers
2016 Value-Based Payment Modifier
The Affordable Care Act requires CMS to apply a VBM to physician payments for all providers by 2017. CMS has been gradually phasing in the VBM program. For 2016, the VBM carries a potential penalty of 4.0 percent for groups of 10 or more providers (eligible providers include all physicians and advanced practice providers, full time and part time). The VBM penalty will be applied to 2018 payments based on 2016 dates of service. The VBM penalty will be avoided if at least 50 percent of the providers within a group satisfy the minimum PQRS reporting requirements in 2016.
CMS is also continuing the VBM scoring methodology, which looks at both cost and quality scoring for individual providers and groups. Failing to meet the PQRS reporting requirements would trigger an automatic 4 percent penalty under the VBM program (see Table 6 for a summary of PQRS penalties). Groups satisfying PQRS reporting go on to the quality-tiering step and will be graded as below average, average, or above average and have the potential to earn a small bonus. Importantly, as MIPS takes over in 2019, VBM is being phased out after 2018.
Other Resources
Resources for these and other topics can be found on the reimbursement section of the ACEP Web site. Mr. McKenzie is also available to field your questions at 800-708-1822, ext. 3233. Finally, ACEP offers well-attended and highly recommended coding and reimbursement educational conferences each January.
Next month, we’ll look at the CMS proposal to eliminate the global surgical package for procedures, 2016 coding changes, an ICD-10 update.
Dr. Granovsky is president of LogixHealth, an ED coding and billing company, and currently serves as the course director of ACEP’s coding and reimbursement courses as well as the Chairman of ACEP’s National Reimbursement Committee. Mr. McKenzie is reimbursement director for ACEP.
Pages: 1 2 3 | Multi-Page






No Responses to “What Emergency Physicians Need to Know about the 2016 CMS Fee Schedule”