The Centers for Medicare & Medicaid Services (CMS) released the Medicare Physician Fee Schedule (PFS) Final Rule on Oct. 30, 2015. It addresses changes to the PFS as well as other important Medicare Part B payment policies. The rule became effective Jan. 1, 2016, and was published in the Nov. 16, 2014, Federal Register.
Explore This Issue
ACEP Now: Vol 35 – No 01 – January 2016Conversion Factor
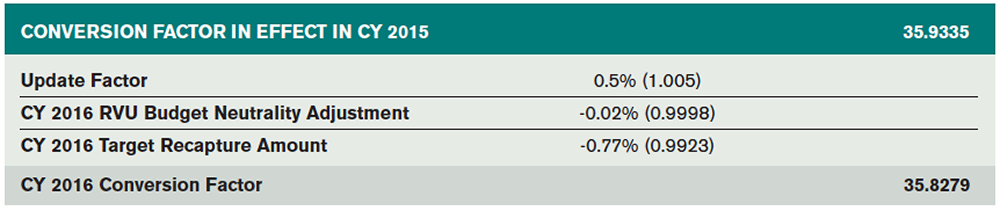
At the conclusion of 2015, the Medicare conversion factor (the amount Medicare pays per Relative Value Unit [RVU]) was set at $35.9335. The 2016 rule is no longer governed by the Sustainable Growth Rate (SGR) formula, which had mandated continuing annual cuts to physician payments, resulting in year-after-year Congressional rescues with short-term fixes. Instead, with the passage of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), signed into law on April 16, 2015, the draconian SGR cuts were permanently repealed and the conversion factor was stabilized. In addition to broad sweeping payment reform related to Physician Quality Reporting System (PQRS), the value-based payment modifier (VBM), meaningful use, and alternative payment models, MACRA provides positive annual payment updates of 0.5 percent through 2019. However, due to two additional pieces of legislation—Protecting Access to Medicare Act of 2014 (PAMA) and Achieve a Better Life Experience Act of 2014, which mandate net cost savings of 1 percent—the final 2016 conversion factor will actually be decreased by 0.3 percent. As a result, the 2016 Final Rule published a conversion factor of $35.8279 (see Table 1).
Merit-Based Incentive Program
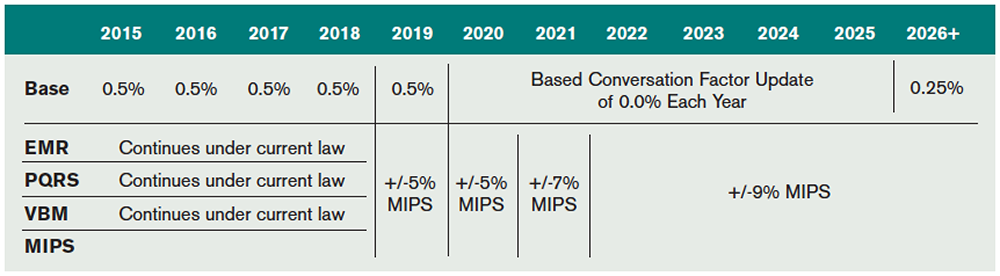
The Merit-Based Incentive Payment System (MIPS) is a new payment mechanism that will provide annual updates to physicians starting in 2019 based on performance in four categories: quality, resource use, clinical practice improvement activities, and meaningful use of an electronic medical record (EMR) system.
Unlike the flawed SGR, the new system will adjust payments based on individual performance. Importantly, MIPS does not set an arbitrary aggregate spending target, which previously led to the need for annual patches to prevent SGR-mandated cuts. The three existing quality programs (PQRS, VBM, and EMR) will be consolidated under MIPS beginning in 2019. An overview of the evolution of the various federal quality programs is in Table 2.
Geographic Practice Cost Index Update
The Geographic Practice Cost Index (GPCI) is used by CMS to modify the RVU values based on regional differences relating to cost of living, malpractice, and practice cost/expense, which allows Medicare to adjust reimbursement rates taking into account regional and practice-specific factors. Some states have a permanently fixed work GPCI, including Alaska at 1.5 and the frontier states (Montana, Nevada, North Dakota, South Dakota, and Wyoming) at 1.0. Other states are subject to a work RVU GPCI that ranges from 0.6 to 1.2. In past years, Congress passed single-year legislation, setting a GPCI work floor of 1.0 that then expired at the end of the year. Section 102 of PAMA allowed for another extension of the work GPCI floor, and the existing 1.0 floor on the physician work GPCI was extended through March 31, 2016.
ED E/M RVUs Stable for 2016
Emergency medicine’s RVU values are stable for 2016, with only small decimal point–level changes. For 2016, the work RVUs for emergency medicine services remain unchanged. The total RVUs (work, malpractice, and practice expense RVUs) associated with ED E/M services 99281–99285 and 99291 will experience small changes driven by adjustments in practice expense and liability expense. The CMS-published specialty-specific impact analysis states that emergency medicine will experience a 0 percent update in overall RVU values for 2016. The 0 percent increase for emergency medicine as a specialty published by CMS contains moderate rounding. Though accurate for 99283, the RVUs for many of the other ED codes are minimally decreased at the hundredth of an RVU level (see Table 3).
Pages: 1 2 3 | Single Page





No Responses to “What Emergency Physicians Need to Know about the 2016 CMS Fee Schedule”