
The emergency department (ED) at Scripps Mercy Hospital San Diego is a different breed of ED. This can be felt upon entering the beautiful southern California facility through the patient entrance. During my visit the greeter area was quiet, uncluttered, and virtually empty at 4 p.m. Seeing more than 76,000 annual visits, this urban academic Level I Trauma Center is a STEMI-receiving hospital, geriatric emergency department (GED) certified, and a Stroke Center.
Explore This Issue
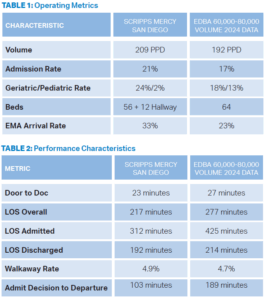
ACEP Now: July 2025Other operating characteristics for this department are seen in Table 1. Interestingly, the geriatric rate is higher than the average for similar departments, and the pediatric rate is lower—both suggesting a higher acuity patient mix—yet the admission rate is only 21 percent. The EMS arrival rate is quite high and this is challenging from an operational standpoint. They have a high behavioral health (BH) population but only modest boarding.
The operations playbook of best practices for EDs in the 60,000–80,000 annual visits volume band is now well recognized and includes the following features:
- a physician in triage (PIT) intake process to ensure the timeliness of the patient/clinician encounter, even during times of surge and high boarding when the department is likely full,
- acuity-based patient care zones with like patients being treated in one area,
- a “fast track” for extremely low acuity patients who may be treated by an advanced practice provider (APP),
- a “mid-track” or vertical care area where middle acuity patients remain vertical to receive diagnostics and therapeutics, and are likely discharged home,
- an acute care or major care area reserving patient beds for the sickest patients that are likely to be admitted, and
- team-based, zone-based care delivery with a care team (physicians, nurses, and techs) all taking care of the same patients in a pod or a zone.
Doing Things Differently
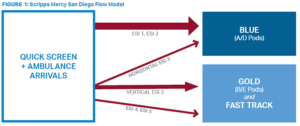
The ED at Scripps Mercy Hospital San Diego does not have a PIT process. Instead, it actively pushes patients into care spaces. The department does have acuity-based care zones. Care is provided largely by teams in acute care zones. That said, the department incorporates floating and flexibility in the name of efficiency: Care of patients in hall beds and in the fast track is shared among all clinicians instead of using dedicated ones in those areas.
In fact, their patient flow model is more typical of a low-volume ED (see Figure 1).
Pages: 1 2 3 | Single Page





2 Responses to “Scripps Mercy Hospital San Diego’s Unique ED Culture Breeds Innovation”
August 3, 2025
Michael Lipscomb, MD, FACEPDear ACEP Now Editorial Team,
Thank you for publishing this great article on the Scripps Mercy Hospital San Diego emergency department. The so-called “secret sauce” of operational best practices is well known to anyone who’s spent time in an ED. What’s much less common and so critical—is true hospital-wide buy-in and the full commitment of ED staff to these principles.
The most impactful elements highlighted were:
1. The hospital’s system-wide commitment to reducing boarding times by prioritizing timely inpatient discharges.
2. Robust ED pharmacist coverage—20 hours a day, per the article.
3. 24/7 critical care support for the ED.
4. Consistent case management presence—12 hours a day.
5. And most importantly, a deeply embedded culture of “patients first,” not “me first.”
I hope hospital administrators and other EDs across the country read this and take note. The more these approaches are adopted, the more we’ll see them become standard practice—and the better care our patients will receive.
Best regards,
Mike
August 3, 2025
Ev FullerKudos for getting hospital leadership to understand the ED’s needs. Looking at this article, 200-ish daily volume with 50+ rooms and 12 hallway beds, as long as the ED is fully staffed and with only a 100 minute delay to get admitted patients upstairs sounds like how EDs are supposed to work. For context, I currently work in an ED with 35 beds and daily volumes of 100-120 so should meet the 4 patients/bed/day standard for ED throughput…BUT…typically holding 15-25 boarders with boarding times often hitting 96 hours. While their flow model is certainly different from an equivalent size ED, I think the CULTURE difference there is that inpatient boarding is recognized as the primary driver of ED congestion and the ED and hospital leadership has prioritized getting admitted patients upstairs to let the ED do ED things.