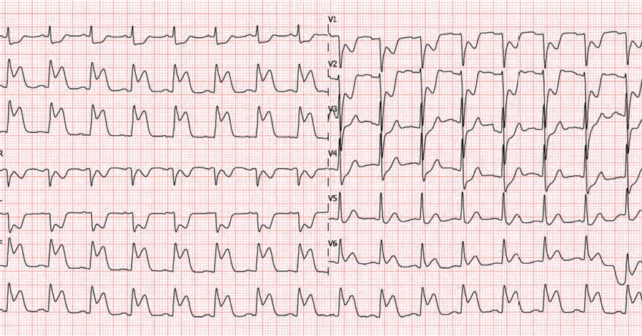
A 64-year-old male collapses after shovelling snow. Paramedics find a patient with eight out of 10 chest pain looking visibly uncomfortable. Vital signs are normal, but the ECG shows ST elevation in the inferior leads and some ST changes in V1-V2 that make you wonder if your patient is having an acute myocardial infarction (MI) with right-sided ventricular involvement (RVMI). In the emergency department, you administer 160 mg of chewable aspirin and your colleague asks if you should also administer 400 ug of nitroglycerin.
Explore This Issue
ACEP Now: Vol 43 – No 03 – March 2024Background
Many of us may have been taught not to give nitrates to a patient with an RVMI. This likely comes from the American Heart Association (AHA) guideline recommendation stating that nitroglycerin is contraindicated in these situations.1 It is categorized as Class III, LOE C (very low-level evidence) but has become part of clinical practice and EMS protocols.
The pathophysiologic rationale was that nitrates would cause vasodilation and thus reduce right ventricular preload, decreasing left end diastolic volume, and ultimately resulting in clinically important hypotension. Many times, pathophysiology has been used to explain something in medicine only to be discovered later that the human body is much more complex than we thought.
The evidence for this recommendation comes from a single retrospective observational study of 40 patients with inferior MIs published in 1989.2 A large portion, 20 patients (50 percent), had hypotension after being administered nitrates. Those with inferior MI and hypotension had ECG evidence of RV involvement. It is important to note that there was no standardization of the nitrate dose or route of administration, so it’s hard to know how to extrapolate the findings to our modern practice and protocols.
Clinical Question
In patients with right ventricular myocardial infarction (RVMI), is nitrate administration associated with increased adverse events compared to patients with myocardial infarctions in other anatomic regions?
Reference: Wilkinson-Stokes M, Betson J, Sawyer S. Adverse events from nitrate administration during right ventricular myocardial infarction: A systematic review and meta-analysis. Emergency Medicine Journal. 2022;40(2):108-13.
- Population: Adult patients diagnosed with an acute MI
- Exclusions: Patients with coronary vasospasm
- Exposure: Nitrate administration in any dose and by any route.
- Comparison: Patients with acute right-sided myocardial infarctions to patients with acute MI involving any other anatomic regions
- Outcome:
- Primary Outcome: Any adverse outcomes reported in the identified literature.
- The primary meta-analysis excluded studies of low quality, but a secondary analysis was also performed including identified studies (2) that were deemed of lower methodologic quality.
Authors’ Conclusions
“This review suggests that the [American Heart Association] and [European Society of Cardiology] contraindications [stating that nitrates are contraindicated in RV MI] are not supported by evidence. Key limitations include all studies having concomitant inferior and RVMI, no evaluation of beneficial effects in any of the studies, and very low certainty of evidence. As adverse events such as hypotension are transient and easily managed, nitrates are a reasonable treatment modality to consider during RVMI on current evidence.”
Results
Their search strategy found five studies that met the inclusion criteria. Of the five studies, two used nitroglycerin 400 μg sublingual as their treatment and could be meta-analyzed. One was a small study (n=46) by McConnell et al, conducted in the UK and had 19 RVMIs. The other was a larger Canadian study (n=1,004) by Robichaud et al and included 86 patients in the cohort with an RVMI.
Key Results
There was no statistical difference observed in adverse events with the administration of nitrates based upon the region of cardiac infarction.
- Primary Outcome: Adverse event rates of combined inferior and RVMI
- Relative risk 1.31 (95 percent CI 0.81 to 2.12)
- Adverse events reported were categorized as transient and minor.
EBM Commentary
- Pillars of Salt and Sand: In the systematic review and meta analysis, the authors point out that the “don’t give nitrates in RVMI patients” recommendation seems to stem from the 1989 Ferguson, et. al., study of 40 patients. That retrospective study reported 20 patients with an inferior MI and hypotension after getting nitrates, and 20 patients with an inferior MI who weren’t hypotensive after receiving nitrates. In the first group (hypotension), 15/20 patients had ECG evidence of RV involvement. Only 2/20 patients in the second group (non-hypotension) had ECG evidence of RV involvement. As is often the case, when you go back to the primary literature that informs guideline recommendations you discover it’s not high-level evidence.
- Papers Meta-Analyzed: Arguably the most compelling study included in the analysis (SRMA) is the one by Robichaud et al (n=1,004).3 It looked at the administration of 400 ug of sublingual nitroglycerin in MI patients who were categorized as inferior MI, inferior plus RVMI, inferior plus other territory, and MI’s involving only non-inferior/RVMI territories. What it demonstrated was that there was no increased risk to any of those subgroups when given nitrates. Interestingly, nitrate administration appeared to be safest in patients experiencing an isolated inferior MI. The other paper meta-analyzed is the other smaller study (n=46) by McConnell et al.4 It was only published as an abstract presented at a conference. The SRMA authors were able to contact the study team, get the original study data, and incorporate that into their meta-analysis. McConnell’s findings are congruent with the larger Robichaud et al study.
- Benefits: The SRMA only looked at the potential harms of administering nitrates to patients with acute MIs. The hypotension observed is often transient, easily managed, and unlikely to be clinically meaningful (i.e., a monitor-oriented outcome). None of the studies included in the SRMA looked at the benefits of nitrate administration such as analgesia balanced against the risks of transient hypotension. The AHA recommends giving patients with ischemic discomfort up to three doses of sublingual or aerosol nitroglycerin until pain is relieved or low blood pressure limits its use (Class I, LOE B). This recommendation is much stronger than the Class III, LOE C provided for the contraindication of nitrates in RVMIs.
Bottom Line
It is reasonable to administer nitrates to patients with an RVMI. Be prepared to manage the potential transient hypotension when giving nitrates regardless of the infarct territory.
Case Resolution
The patient is having eight out of 10 chest pain and the ECG suggests an inferior MI with possible right ventricular involvement. You know the latest evidence doesn’t support the contraindication of nitroglycerin administration and that it might ease his pain. At the same time, you know that any patient with an MI might become hypotensive, so before providing the first spray of nitroglycerin you establish an intravenous line.
Thank you to Dr. Rupinder Sahsi who works as an emergency physician in Kitchener-Waterloo, Ontario, Canada and is an assistant medical director for EMS at the Centre for Paramedic Education and Research in Hamilton, Ontario, Canada for his assistance with this critical appraisal.
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.
References
- Neumar RW, Shuster M, Callaway CW, et al. Part 1: Executive summary. Circulation. 2015;132:S315–67.
- Ferguson JJ, Diver DJ, Boldt M, et al. Significance of nitroglycerin-induced hypotension with inferior wall acute myocardial infarction. Am J Cardiol.1989;64:311–4.
- Robichaud L, Ross D, Proulx M-H, et al. Prehospital nitroglycerin safety in inferior ST-elevation myocardial infarction. Prehosp Emerg Care. 2016;20:76–81
- McConnell AH, Davis M, Van Aarsen K, et al. LO33: prehospital adverse events associated with nitroglycerin use in STEMI patients with right ventricle infarction. CJEM. 2017;19:S39.
Pages: 1 2 3 | Multi-Page




3 Responses to “Revisiting Nitroglycerin in MI with Right-Side Ventricular Involvement”
March 10, 2024
Joseph Shiber, MDYou have missed the big picture. NTG will cause venodilation in every patient. If they are dependent on RV filling for contraction as during myocardial ischemia/infarction then you will expect this effect to be pronounced. It’s not that you can’t give NTG for the anti-anginal effect of potentially pain relief (that’s all the benefit you will ever get from NTG unless there is actual coronary artery spasm w/o complete coronary occlusion/thrombosis) but you need to be ready to intervene by stopping the NTG (it should be IV and not SL or topical since you need the effect to go away quickly) and give an IVF bolus. If you give a SL NTG and do not have IV access yet to give an IVF bolus, you will never forget this mistake even if the patient hopefully doesn’t arrest.
March 10, 2024
Andrew SchareAnother question to ask is why do we give nitrates at all to patients with acute myocardial infarction. There is no benefit to morbidity or mortality.
May 14, 2025
JCPhilUmmm… Dare I say, pain?