Explore This Issue
ACEP Now: Vol 36 – No 06 – June 2017(click for larger image)
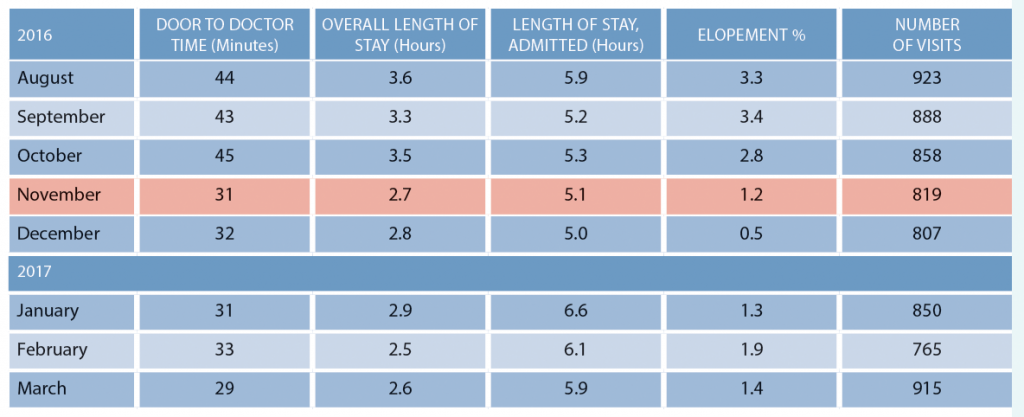
Table 1: Houlton Regional Hospital Metrics Before and After Implementing Patient Flow Changes in November 2016
Re-Engineer Flow for High Flow and Low Flow
The leadership also articulated a process for times of the day when all nine beds are full (high flow).3 During these times, the provider sees new patients in the RTU (one specified chair) until beds are available. Diagnostic testing is started, and patients are managed in the waiting room until treatment spaces open up. Emergency Severity Index 1 and 2 patients are accommodated in the main emergency department by moving less-acute patients out.
Develop a Night Plan with the Hospitalists
Finally, like many rural hospitals, the department struggled with on-call coverage at night. The heavy lifting was being done by the hospitalists, who admitted the majority of patients. However, the hospitalists were working seven days straight and were wearing out quickly. The hospitalists needed to have a few hours on the night shift to get sleep, but the emergency department wanted to get its patients bedded down on the inpatient units. The solution was the implementation of “holding orders,” also known as “bridge orders” or “timed-out orders.”4
The before and after data in Table 1 are very impressive.
Hats off to the Houlton Regional leaders. When you think you can’t take your emergency department to the next level of operational performance, just remember “The Maine Thing.”
References
- Welch S, Davidson S. Exploring new intake models for the emergency department. Am J Med Qual. 2010;25(3):172-180.
- Augustine J. ‘Pull to full’ speeds up flow. ED Manag. 2011;23(3):30-31.
- Welch S, Savitz L. Exploring strategies to improve emergency department intake. J Emerg Med, 2012;43(1):149-158.
- Traub SJ, Temkit M, Saghafian S. Emergency department holding orders. J Emerg Med. 2017; pii: S0736-4679(17)30110-5.
Pages: 1 2 | Single Page






One Response to “Patient Flow Improvements to Boost Efficiency in Small Emergency Departments”
July 5, 2017
ToddI am surprised how casually bridge orders are mentioned as a component to improving ED throughput.
ACEP explicitly has a written policy discouraging this practice, and rightfully so:
https://www.acep.org/Clinical—Practice-Management/Writing-Admission-and-Transition-Orders/