Explore This Issue
ACEP Now: Vol 35 – No 10 – October 2016(click for larger image)
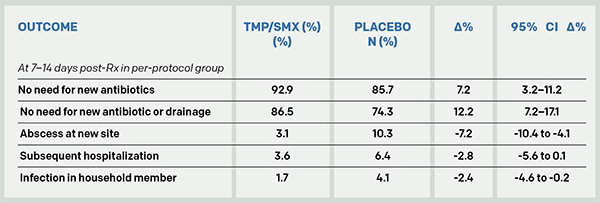
Table 1: Outcome of Patients with a Drained Skin Abscess Randomized to TMP/SMX or Placebo
So do we now abandon, “Just say ‘no’ to antibiotics for abscesses,” and risk promoting bacterial resistance Armageddon? There’s another perspective to these results. Most patients recover with drainage alone, 85.7 percent not needing a new antibiotic and 74.3 percent not needing either a new antibiotic or more drainage. Further, the placebo group was found to be at no increased risk of subsequent rare invasive infections.
I asked an emergency medicine antibiotic stewardship expert, Larissa May, MD, MSPH, MSHS, at the University of California, Davis. She replied, “I would argue that these results cannot be generalized to truly uncomplicated abscesses as a substantial minority of participants fell into the moderately ill category (diabetes, systemic signs of infection, and abscesses >75 cm2). I am more likely to treat patients who suffer from repeated infections. In addition, even if the study reinforces the current practice of prescribing antibiotics to most patients with uncomplicated abscesses, there is opportunity for decreasing duration of antibiotic use. The authors chose seven to 10 days, which is not necessary.”
Emergency physicians are routinely second-guessed when complications occur, so I asked an infectious diseases expert, Brad Spellberg, MD, at Los Angeles County-University of Southern California Medical Center, who advises the US Food and Drug Administration on antibiotic trials, about his take. He replied, “I cannot understand people’s fixation on not giving antibiotics to people we know have bacterial infections, but they seem to be perfectly at ease blasting people with viral bronchitis, sinusitis, otitis, etc. with pseudomonally active therapy, typically with vanco. … Patients with abscesses need to be treated. … Your data have frankly made it below the standard of care not to do so.”
Brad, we caught the dig about our vosyn abuse. Ouch. We’ll keep working on that.
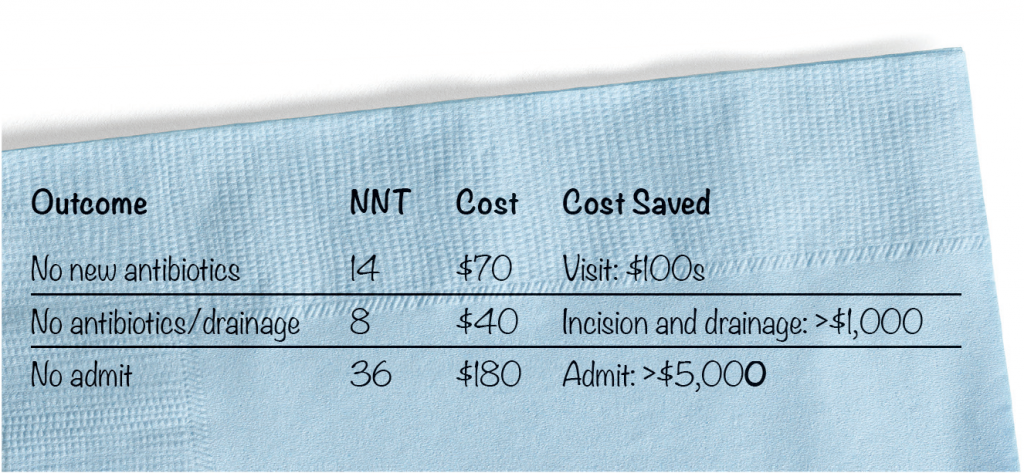
A seven-day course of TMP/SMX costs about $5 on GoodRx.com. Here’s a back-of-the-napkin cost analysis (see Figure 1).
(click for larger image)
Figure 1. Back of Dave’s Napkin: Number Needed to Treat (NNT) and Cost/Savings to Prevent One Failed Case
With an antibiotic that is so cheap, routine use is cost-saving, even with a small outcome benefit considering the savings in avoiding a return visit and especially an extra drainage procedure or hospitalization.
“I cannot understand people’s fixation on not giving antibiotics to people we know have bacterial infections, but they seem to be perfectly at ease blasting people with viral bronchitis, sinusitis, otitis, etc. with pseudomonally active therapy, typically with vanco. … Patients with abscesses need to be treated. … Your data have frankly made it below the standard of care not to do so.” —Brad Spellberg, MD, at Los Angeles County-University of Southern California Medical Center
Jerry Hoffman, MD, perhaps emergency medicine’s toughest literature critic, concluded, “I was quite surprised by the results … and actually wished they’d been different. But this is very good evidence, and certainly the best we have, of a small but real benefit. So it strongly suggests that a few days of antibiotics is worth it.” This new evidence at least opens the door to a discussion with your patient.
Pages: 1 2 3 | Single Page





No Responses to “Antibiotic Therapy for Abscesses Medical Dogma Challenged by Evidence-Based Research, Outcomes”