After a three-year saga of flawed public policy, difficult politics, and dangerous regulations, Washington Chapter ACEP is proud to report the success of the “ER is for Emergencies” program, which has achieved unprecedented results. It started in 2010 with a legislative mandate borne out of the necessity to save money in the state budget as a result of the recession. The Washington State Health Care Authority (HCA) proposed a $36 million annual savings through a policy to “just not pay” after the third ED visit judged to be nonemergent in 12 months. Calling ED providers “poor stewards of the health care dollar” in print and making a direct threat to prudent layperson protection, the HCA then went on to create a nonemergent list of 700-plus diagnoses, which included chest pain, hemorrhage with miscarriage, and sudden loss of vision. Despite our attempts to work with the regulators, litigation became the only option to stop the dangerous proposal.
Explore This Issue
ACEP Now: Vol 33 – No 07 – July 2014Washington Chapter ACEP stepped up by engaging more than 90 percent of our providers to create the Washington State Emergency Medicine Action Fund and file suit. National ACEP and the Emergency Medicine Action Fund provided financial support for litigation and experienced researchers to provide data on the dangers. We brought allies including the Washington State Medical Association, Washington State Hospital Association, other physician specialties, and patient advocacy groups. The providers won the battle in court but were committed to helping the state improve care and save money.
A Solution Where Everyone Wins
This was the turning point. While the HCA pushed back, the legislature sought solutions and asked for our ideas. We established ground rules of preserving access to emergency care; protecting the prudent layperson standard; and delivering high-quality, cost-effective care. We realized we first had to invest some money in infrastructure and then build a system around communication. Through advocacy in the capital and the governor’s mansion, an aggressive public relations effort, and tenacity, the legislature passed Bill 2127, creating the Washington State Seven Best Practices:
Emergency Department Utilization: Update on Assumed Savings from Best Practices Implementation, March 20, 2014
1. Tracking of ED visits, with an automated notification sent to providers of any patient visiting five or more times in the last 12 months. All hospitals have adopted the program. This tracking includes a summary of prior visits, care plans from any facility in the state, and safety warnings such as violence or radiation alerts.
2. Implementation of an education program for all providers, administrators, and patients via forums, webinars, handouts, and posters in ED waiting rooms (see the January 2014 issue of ACEP Now for more on these posters).
3. Identification of the highest utilizers, along with follow-up and care plans for them. This population had significant issues, including 86 percent with mental health issues and 41 percent with addiction issues. The key for these patients was an emphasis on case management with care plans and coordination with primary care.
4. A requirement that “frequent flyers,” or overutilizers, are seen by primary care within 72 hours.
5. Creation of a statewide narcotics program. A 17-point program was adopted by all ED providers that created a statewide standard for prescribing opioids for chronic, noncancer pain.
6. A requirement that providers enroll in the prescription-monitoring program (PMP). Despite 96 percent enrollment, the reality is that the current data pull system is difficult to use. Thus, this summer, the PMP data will be pushed through the Emergency Department Information Exchange system. This eliminates the pull method and the inherent bias in provider selection.
7. Creation of a feedback system to track success for both the HCA and individual departments and their providers.
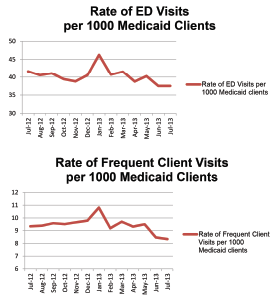
The first-year results of this effort exceeded everyone’s expectations. A full report is available at http://www.hca.wa.gov/Documents/EmergencyDeptUtilization.pdf. Highlights include a 9.9 percent reduction in overall ED Medicaid visits and a 10.7 percent reduction among frequent utilizers. The ER is for Emergencies campaign resonated, and our low-acuity visits dropped 14.2 percent.
What about opioid-overdose deaths? We reduced narcotic prescriptions from the EDs 24 percent! This contributed to Washington being one of several states to decrease opioid-related deaths annually for the last three years. Finally, in what began as a budget-generated policy, we saved the state more than $34 million and counting.

Emergency Department Utilization: Update on
Assumed Savings from Best Practices Implementation, March 20, 2014
The economics of health care are changing, but the foundation of preserving access to care should remain paramount. With expanding Medicaid enrollment, many states will be trying to rein in costs, and Washington’s solution is an option for significant savings. The Centers for Medicare & Medicaid Services recently moved to protect the prudent layperson standard by preventing Florida from enacting a visit limit.
ACEP must continue to be where all of health care looks for solutions. The way to solve issues is through innovation and building alliances. Seven Best Practices proved we can—but we cannot rest on our successes. With dramatic changes in health care on the horizon, opportunities abound for ACEP to continue to lead.
Dr. Anderson is past president of Washington Chapter ACEP.
Dr. Schlicher is secretary, treasurer, and legislative chair of Washington Chapter ACEP.
Pages: 1 2 3 | Multi-Page





No Responses to “7 Best Practices to Reduce Emergency Department Misuse”