
The Centers for Medicare and Medicaid Services (CMS) has released the 2025 Physician Fee Schedule (PFS) Proposed Rule, which will affect emergency medicine reimbursement significantly. Following a commentary period lasting until September 9, 2024, CMS is expected to issue its final PFS rule in early November, which will impact services beginning January 1, 2025.
Explore This Issue
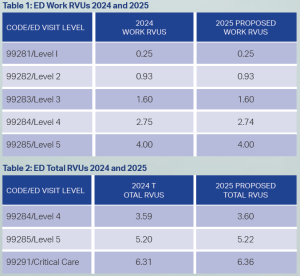
ACEP Now: Vol 43 – No 10 – October 20242025 Work RVUs Hold Steady
Acting to protect the safety net, ACEP’s RVS Update Committee (RUC) members continually advocate for the recognition of the complexity of our day-to-day bedside care. The ACEP RUC team has been very successful in protecting our work RVUs.
2025 Total RVUs Small Possible Increase
Due to small potential increases in the calculation of Practice Expense, emergency medicine may see a roughly ½ percent increase in Total RVUs for certain key codes.
The Medicare payment per RVU (the conversion factor) is unfortunately dependent on the AMA and the entire House of Medicine successfully convincing Congress to increase the budget for Medicare Part B, which governs payment for physician services. For 2025, CMS proposes a Medicare PFS conversion factor of $32.3562, a 2.8 percent decrease from the 2024 conversion factor of $33.2875. The 2025 proposed rule, as in past years, is subject to “budget neutrality,” a previously obscure factor which is becoming increasingly impactful. The 2024 budget neutrality adjustment was partially offset by 2.93 percent due to a funding patch passed by Congress through the Consolidated Appropriations Act. Unfortunately, the 2024 2.93 percent “patch” was only for one year and was not included in the 2025 proposed CMS calculations.
What Is Budget Neutrality?
The budget neutrality induced potential 2025 decrease is due to the CMS decision to increase reimbursement for the office visit codes back in 2021, a boon for urgent cares, which report physician services using office codes. Due to an historic clause in the payment and budgetary regulations, increases in Medicare part B spending beyond $20 million must be offset by decreases to the conversion factor to keep Medicare expenses in check. Unfairly, there is no indexing to inflation, so although expenses continually increase, Medicare payments are not keeping pace.
Due to the budget neutrality adjustment in the conversion factor, the whole House of Medicine could see a 2.8 percent decrease in payments per RVU for 2025. ACEP has mounted a vigorous campaign to protect the safety net and is urging Congress to stabilize the conversion factor for 2025 and index future physician reimbursement to inflation. 2025 Update to the Merit-Based Incentive Payment System (MIPS) The Merit-Based Incentive Payment System (MIPS) represents a payment mechanism that provides for annual reimbursement adjustments related to quality program requirements impacting 2027 payments based on 2025 performance in four categories.
In an advocacy win, CMS is proposing to keep the penalty threshold at 75 points (rather than the previously considered 82 points) due to significant feedback related to the complexity and challenges of the MIPS program.
MIPS Value Pathways
2025 is the third year in which a new reporting option in MIPS called MIPS Value Pathways (MVPs) is available. MVPs represent an approach that will allow clinicians to report on a more clinically integrated set of quality measures built around a specific emergency medicine episode or acute care condition. ACEP developed an emergency medicine-focused MVP that became available in 2024. The ACEP MVP is called “Adopting Best Practices and Promoting Patient Safety within Emergency Medicine.” More information about the MVP is available here.
ED Continued Traction with Telehealth Services
CMS has been continually examining which codes placed on the list of approved Medicare telehealth services during the COVID-19 public health emergency should be continued. The current CMS process involves a list of “provisionally” approved codes, which include 99281-99285. The 2025 Proposed Rule is silent to the issue of sunsetting the ED codes, so they are likely to remain provisionally approved for telemedicine for 2025.
For more information regarding pressing ED reimbursement issues, attend the ACEP Reimbursement and Coding Conference in Orlando, Fla., January 20-22, 2025.
 Dr. Granovsky is president of LogixHealth, an ED coding and billing company, and currently serves as the course director of ACEP’s Coding and Reimbursement courses. He may be reached at mgranovsky@logixhealth.com.
Dr. Granovsky is president of LogixHealth, an ED coding and billing company, and currently serves as the course director of ACEP’s Coding and Reimbursement courses. He may be reached at mgranovsky@logixhealth.com.
Pages: 1 2 | Multi-Page





One Response to “2025 Physician Reimbursement Update”
October 20, 2024
Stephen EpsteinA couple of the finer details (though Dr. Granovsky is the real expert here) –
First, the MIPS Value Pathway for emergency medicine includes the “foundation layer” in which an EM group must choose a population health measure. The choice is between hospital-wide, 30-day, all-cause unplanned readmission rate or risk-standardized hospital admission rates for patients with multiple chronic conditions. Neither is a particularly good option.
Second, the emergency medicine cost measure will be used for the first time this year and will comprise 30% of the overall MIPS score. While this new measure field-tested well, it throws another unknown into a group’s ability to predict how they will ultimately score on MIPS.
Third, ACEP isn’t going alone on the advocacy front – the AMA has made a big push for an annual inflationary update to the physician fee schedule. Together, those efforts have led to a majority of the House of Representatives requesting action: https://www.documentcloud.org/documents/25210928-physician-fee-schedule-letter.
Finally, we are awaiting the publication of the latest RAND study on the value of emergency medicine, which might also be beneficial in ACEP’s advocacy efforts for fair payment.