
The newly designed flow model also involved the creation of small internal waiting rooms (see Figure 2) to keep patients moving forward, with a goal of never sending them back to the main waiting room.
Explore This Issue
ACEP Now: Vol 37 – No 01 – January 2018Finally, a front flow facilitator monitored flow into the department and kept things moving in the front of the department, while a back flow facilitator monitored flow in the major care areas and into the hospital. These highly trained and experienced nurses performed no direct patient care but rather functioned like air traffic controllers, making sure that flow into and out of the department was smooth and efficient.
The Results
The results were astounding. First, the productivity of the minor care areas more than doubled. The variation was proportional to the ESI breakdown of arrivals that 24-hour cycle (see Table 1).
Then in terms of measured operational performance, the new model really rocked. The VCU emergency department is now posting median wait times to see the physician of fewer than 10 minutes and walkaway rates of less than 1 percent (see Table 2).
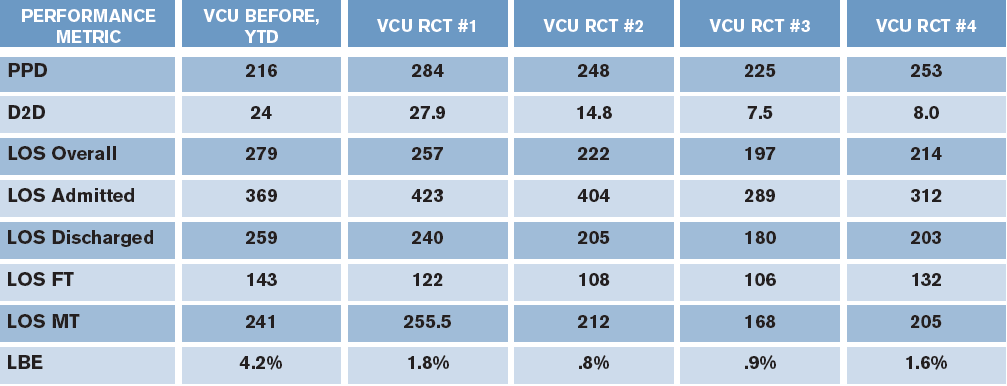
(click for larger image) Table 2. Pre- and Postimplementation Performance Metrics
RCT=rapid cycle test; PPD=patients per day (24-hour period); D2D=door-to-doctor time; LOS=length of stay; FT=fast track; MT=mid track; LBE=left before examination
Most departments of such high volume, with teaching missions and tertiary care delivery, find it hard to achieve this kind of performance. By engaging the physicians and staff early and delegating pieces of this global improvement project to individuals, they moved the entire department forward. The VCU leadership team refused to accept mediocre metrics, and together it put its vision in action!
Pages: 1 2 | Single Page







2 Responses to “Virginia Commonwealth University Improves Patient Flow Through “Vision in Action” Model”
January 22, 2018
Peter RizzoThere is concern of scope creep in this; why can’t the doctor at triage order tests? This established a huge bias at beginning of work up. I’d like to see if a physician at triage could only make decisions on resource management alone. However, I’m sceptical of people “wasting” that doctor as a secondary triage.
March 1, 2018
Shari WelchHello Peter,
I think the best results for physician in triage are seen when the physician is resourced to begin work-ups in triage. If all he does is determine the patient’s level of care and zone, sending patients back to the waiting room, you do not gain much in terms of time shaved off the LOS. You are playing to the metric. The only exception would be if the physician determines the stream and the patient is immediately bedded and a SWARM model employed to begin care in the back.
If you put the patient and physician together in triage for quick streaming and then send the majority back to the waiting room, you will not optimize the pIT model. You will be playing to the metric, but not shortening LOS or decreasing walkaways and patient satisfaction will not change much. That is what VCU saw. They had short D2D but high walkaways, a full waiting room and poor patient flow. When PIT was properly resourced everything changed and improved!
S