
As our overall population ages and people live longer than ever, the need for specialized care for older adults in the emergency department is increasing. By 2034, the U.S. Census Bureau projects that older adults will exceed the number of children for the first time in U.S. history.1 Nearly every ED shift includes caring for older patients who present with multiple medical problems, sometimes coupled with social and physical needs. Within the last decade, hospitals started to realize that “one-size ED” does not fit all. This growing population of older adults has unique needs that require special consideration.
Explore This Issue
ACEP Now: Vol 40 – No 02 – February 2021Raising the Standard of Care
ACEP developed its Geriatric ED Accreditation (GEDA) program in 2018, but the work started years prior. In 2013, ACEP, the Society for Academic Emergency Medicine (SAEM), the American Geriatrics Society (AGS), and the Emergency Nurses Association (ENA) released the Geriatric Emergency Department Guidelines, the product of two years of consensus-based collaboration. The guidelines specify broad domains and recommend measures ranging from geriatric-friendly equipment to geriatric-focused staff to more routine screening for delirium, dementia, falls, and more.
These guidelines were used to develop the GEDA framework, featuring three levels of accreditation focused on four key best practices:
- Ensuring geriatric-focused education and interdisciplinary staffing
- Providing standardized approaches to care that address common geriatric issues
- Ensuring optimal transitions of care from the emergency department to other settings (inpatient, home, community-based care, rehabilitation, long-term care)
- Promoting geriatric-focused quality improvement and enhancements of the physical environment and supplies
“Hospitals were trying to address this growing need in patient care on their own. The GEDA program made it easier to identify gaps and areas for improvement; GEDA provides the framework to help facilities get the resources needed to make more formal changes to improve care for older adults,” said Kevin Biese, MD, MAT, FACEP, chair of the ACEP program and co-director of geriatric emergency medicine at the University of North Carolina School of Medicine in Chapel Hill.
The accreditation requirements address staffing, education, policies and procedures, quality, outcomes, equipment, and the right environment—all of which can enhance care for older adults. Take the environmental category requirements for Level 1 accreditation, for example: Simple measures such as dimmed lights, thicker mattresses, and nonslip floors can go a long way to improving patient care.
In most cases, having a geriatric ED does not mean creating a separate space for older adults but rather optimizing processes (screening for geriatric syndromes), physician and nurse education, structural enhancements (appropriate beds, floors, lighting), and community connections to better care for older adults.
In the two and a half years since its inception, the number of hospitals accredited by GEDA has grown rapidly. As of January 2021, GEDA had accredited 219 sites across 35 states and four countries (see Figure 1).
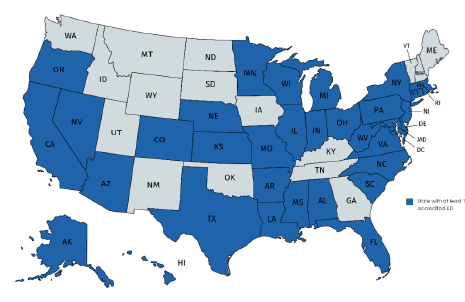
Figure 1: States with GEDA-Accredited EDs
By the Numbers
In January, there were 212 GEDA-accredited sites:
![]()
GEDA is actively working with 350 additional sites seeking accreditation, including working with many health systems and a nationwide project with Veterans Affairs (VA) to accredit more than 60 VA facilities. This growth was made possible through support from the Gary and Mary West Health Institute and The John A. Hartford Foundation to enhance geriatric emergency care across the country.
Beyond Accreditation
Clinical Tools
ADEPT (for Assess, Diagnose, Evaluate, Prevent, and Treat) is a point-of-care tool for managing confusion and agitation in elderly patients. It’s free for all ACEP members and can be accessed here or by downloading the emPOC app, which includes ADEPT as one of its many point-of-care tools. The app is especially convenient for those who have trouble accessing Wi-Fi in their emergency departments and want reliable access to these care pathways.
Click here for a collection of resources including the geriatric ED guidelines, a series of videos about the unique circumstances of geriatric care in the emergency department, and a related eCME bundle.
Networking
Emergency physicians interested in bettering care for older patients can get involved by joining ACEP’s Geriatric EM Section. Joining the section provides opportunities to become a leader in the area of geriatrics. Learn how to get involved and view helpful resources developed by the section.
Ms. Tidwell is GEDA program manager at ACEP.
Ms. Grantham is ACEP’s communications manager.
Reference
- Vespa J, Armstrong DM, Medina L. Demographic turning points for the United States: population projections for 2020 to 2060. United States Census Bureau website. Accessed Jan. 21, 2021.
Pages: 1 2 | Multi-Page




No Responses to “Use ACEP’s Geriatric Resources to Improve Care for Older Adults”