The best questions often stem from the inquisitive learner. As educators, we love, and are always humbled by, those moments when we get to say, “I don’t know.” For some of these questions, you may already know the answers. For others, you may never have thought to ask the question. For all, questions, comments, concerns, and critiques are encouraged. Welcome to the Kids Korner.

Explore This Issue
ACEP Now: Vol 36 – No 04 – April 2017Question 1: In children with acute gastroenteritis (AGE), is there a particular serum bicarbonate level that strongly predicts admission or outpatient treatment failure?
While most AGE literature evaluating serum bicarbonate focuses on its incorporation into assessment scores of dehydration, few studies evaluate its ability to predict hospital admission.
A prospective observational study evaluated 206 children with AGE between the ages of 1 month and 5 years. Of these kids, 59 of 206 (29 percent) had blood work drawn.1 The goal of the study was to assess the validity of the clinical dehydration scale (CDS), which classifies dehydration as “no,” “some,” or “moderate/severe” dehydration. The authors, a priori, grouped serum bicarbonate levels into two groups (< 18 and ≥ 18 mEq/L). In the group with “moderate/severe” compared to “some” dehydration, the serum bicarbonate was < 18 mEq/L in 75 percent versus 39 percent (P=0.22), respectively. This difference was not statistically significant, and there were only a very small number of “moderate/severe” dehydrated patients. The rate of admission was 5 percent (10 of 206), but no comparison was made between admitted and discharged patients. Overall, the study suggested that, as expected, children with worsening dehydration may have lower serum bicarbonate levels.
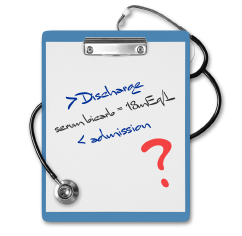
ILLUSTRATION: Chris Whissen PHOTOS: shutterstock.com
Another prospective observational study by Madati and Bachur evaluated 130 children age 3 months to 7 years with AGE.2 Patients received either blood work or an end-tidal carbon dioxide (ETCO2) reading. Per the authors, an ETCO2 of 31 mmHg approximates a serum bicarbonate of 15 mmol/L. In this study, they also confirmed that an ETCO2 of 31 mmHg or less had 98.6 percent sensitivity for demonstrating a serum bicarbonate of ≤16 mmol/L. Regarding admission, they found there was no significant difference in serum bicarbonate values (P=0.11) between patients admitted (17.5 ± 3.3 mmol/L) versus discharged (19.0 ± 3.1 mmol/L). Twelve percent of the patients were admitted.
A study by Freedman et al may best address this topic.3 It’s a secondary analysis of prospectively collected data. In the initial study, the authors were looking at regular versus rapid rehydration. Children were randomized to either a single 20 mL/kg bolus or three boluses (total of 60 mL/kg) over the course of an hour. The primary outcome was whether a serum bicarbonate level could predict an ED revisit within seven days. The study included 226 children older than 3 months of age with AGE and found that 52 of 226 (23 percent) were admitted at the time of initial presentation. Of the remaining discharged patients, 30 of 174 (18 percent) had an ED revisit within seven days. There was no statistically significant difference (P=0.25) between serum bicarbonate values in children who did and did not have a “successful discharge” (not admitted at initial visit and not having a return ED visit within seven days).
Pages: 1 2 3 | Single Page





No Responses to “Treatment for Acute Gastroenteritis, Acute Epididymitis in Pediatric Patients”