While many of us are familiar with spontaneous coronary artery dissection (SCAD) as a common cause of myocardial ischemia in young people, traumatic coronary artery dissection (TCAD) is a rare, potentially life-threatening diagnosis that is challenging to diagnose and often missed in the emergency department (ED), as the clinical features overlap with more common diagnoses that result from blunt chest trauma.1 It is important to pick up this diagnosis early, as emergency treatment with percutaneous coronary intervention (PCI) to restore blood from to the heart can be lifesaving. In this ACEP Now column, I hope to elucidate some of the key clinical clues of TCAD to maximize your chances of picking it up in your blunt chest trauma patients.
Explore This Issue
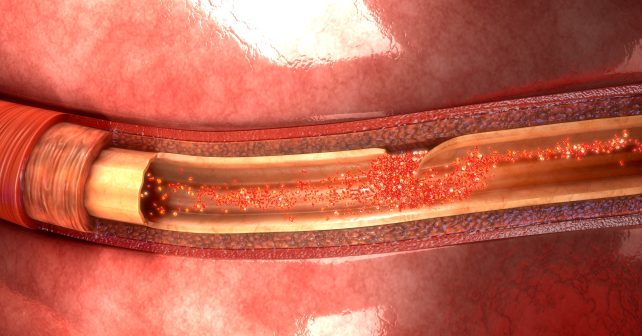
ACEP Now: Vol 43 – No 11 – November 2024TCAD occurs as a result of rapid deceleration, which increases shear forces on the endothelium of the coronary artery. The stress of the traumatic event causes an acute increase in blood pressure. The combination of shear forces on the coronary artery endothelium and sudden increase in blood pressure results in TCAD. The dissection of the coronary artery that occurs in TCAD may lead to thrombus and/or vasospasm resulting in myocardial infarction and all of its potential complications, including death. Aortic dissection as a result of blunt trauma is often immediately fatal, and if patients do survive to be transported to the ED, it can be difficult to diagnose. By contrast, traumatic aortic dissection does not cause cardiac ischemia like TCAD typically does.
There are several reasons TCAD is often missed in the ED besides it being a rare entity with an incidence of only 0.1 percent.2 First, TCAD may result from a relatively low energy mechanism such as a seemingly innocuous blow to the chest in sport. Second, it is predominately diagnosed in young people; 82 percent of patients with acute myocardial infarction after chest trauma are under 45 years of age.3 Another reason TCAD is easily missed in the ED is that the most common cause of TCAD is a motor vehicle crash caused by deceleration and traction or direct impact, and concurrent traumatic injuries in these cases often overshadow the diagnosis.4 Patients may present with altered mental status, rendering them unable to convey symptoms of cardiac ischemia. Generalized chest pain has a broad differential diagnosis in the polytrauma patient. Other cardiac injuries are often considered first, such as cardiac contusion, dysrhythmias, and cardiac tamponade. Finally, symptoms of TCAD may not present for several hours, days, or weeks after the inciting traumatic event, as the rate of expansion of the false lumen may vary considerably.5
Pages: 1 2 3 | Single Page





One Response to “Traumatic Coronary Artery Dissection Diagnosis Tips”
November 23, 2024
Brian Levyanother great short to the point article, Anton Thanks.