Diagnosis
Is your bedside exam reliable? While we are taught about the classic findings of pain with passive stretch, a tense/firm compartment, swelling, focal motor/sensory changes, and decreased pulses, these are not always present and have poor sensitivity.3-5,14,19 Digital palpation has a sensitivity under 50 percent for detection of compartment syndrome affecting the hand and under 25 percent for the leg.22,23 Paralysis and absent pulses are rare, and palpating a tense or firm compartment is not reliable. Swelling of the affected area may be present in only half of patients.3,14,19 Table 2 demonstrates the sensitivity and specificity of exam findings.19
Explore This Issue
ACEP Now: Vol 38 – No 10 – October 2019As you can see from Table 2, many classic findings are highly specific but poorly sensitive.
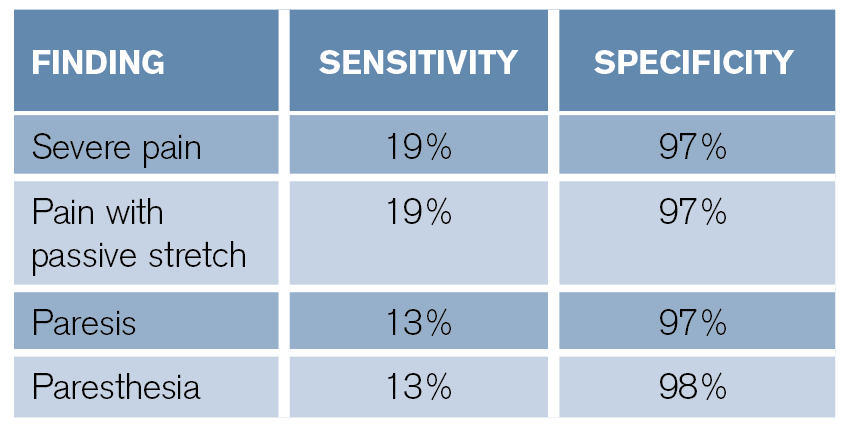
Table 2: Diagnostic Accuracy of Exam Findings19
What happens if you combine signs and symptoms? A combination of pain with passive stretch, pain at rest, and paresthesias has a sensitivity of 93 percent for diagnosis, and the addition of paresis increases sensitivity to 98 percent.19 However, do not rely on the absence of any classic isolated findings. Other items that complicate diagnosis based on history and exam include clinician inexperience, sedation, polytrauma, and intoxication.8,19,24,25
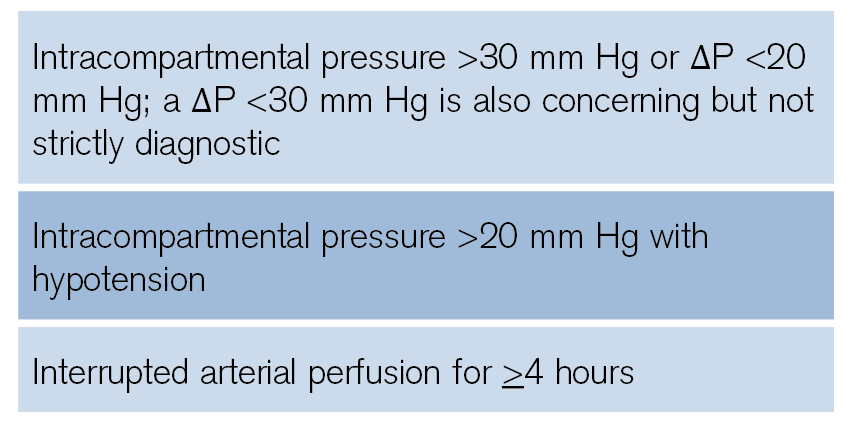
Table 3: Clinical Signs Suggestive of Compartment Syndrome
What about other tools? Abnormal pulse oximetry may indicate compartment syndrome.3,18,19 However, you cannot use this to exclude the condition. Rhabdomyolysis is present in up to 40 percent of patients with compartment syndrome, so be sure to check creatine kinase levels, renal function, and electrolytes.26-28
The most reliable bedside data can be obtained by measuring intracompartmental pressure. Options include a solid-state transducer intracompartmental catheter (STC) device (eg, a Stryker monitor) or other needle manometer/arterial line setups.4-6,19 The Stryker monitor has a diagnostic sensitivity around 95 percent, with specificity greater than 98 percent.29-31 Make sure to place the catheter within 5 cm of the fracture/injury level. However, the catheter tip should be outside the actual site of the fracture. Also ensure the pressure transducer and catheter tip are at the same height.24,32-35

Figure 1: Stryker intracompartmental pressure monitoring device. To measure the pressure in a particular compartment, set the device to zero, insert the needle into the compartment and perpendicular to the skin, inject 0.3 mL sterile saline, and read the pressure displayed on the screen.

Figure 2: Stryker intracompartmental pressure monitoring device being inserted into the lower leg.
Pages: 1 2 3 4 | Single Page





3 Responses to “Tips for Quickly Diagnosing Compartment Syndrome”
November 19, 2019
Emil Pajek MDCannot find the CME that is listed in the article.
ALSO the article in the magazine has DIFFERENT Title than here …cannot find the CME /article or reference.
I had to call the ACEP
February 4, 2020
David GlassSame. I can’t find the CME link / test.
March 20, 2021
J WellsI think you mean AP is diastolic pressure minus compartment pressure