
Explore This Issue
ACEP Now: Vol 41 – No 04 – April 2022(click for larger image)
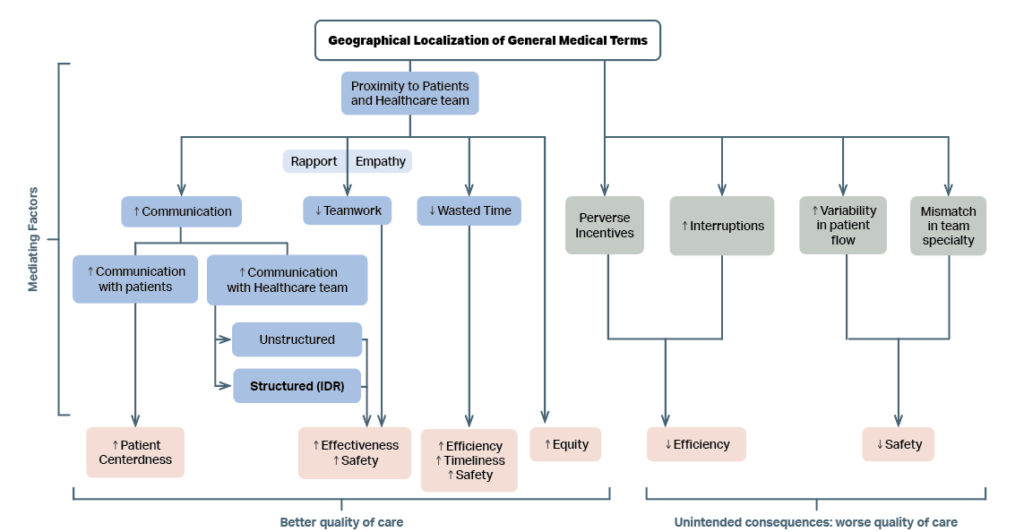
FIGURE 1: Conceptual model depicting impact of geographical localization of general medical teams on quality of care. Mediating factors that lead to better quality of care are described in blue boxes. Mediating factors that are unintended and lead to worsening quality of care are described in grey boxes. The impact on domains of quality of care is described in pink boxes. ‘↑’ indicates an increase; ‘↓’ indicates a decrease; IDR = Interdisciplinary Rounds.
Singh S, Fletcher KE. A qualitative evaluation of geographical localization of hospitalists: how unintended consequences may impact quality. J Gen Intern Med. 2014;29(7):1009-1016.
Geographic localization has been coupled with another innovation: separating the admitting role and the rounding role for hospitalists. Thus, the “triagist” role was born: One hospitalist will admit a patient (the triagist), while another subsequently manages care. Separating these roles improved efficiency and throughput.9 The triagist role allows the patient to be admitted in a timely fashion, and placed on the right unit and team later on. Another related improvement has been the multidisciplinary rounds, particularly those that focus on the discharge of the patient. Geography makes those team rounds more feasible. 10
Another strategy which optimizes hospital throughput involves adjusting the work schedules of hospitalists.11 Schedules that promote continuity were associated with lower mortality, lower readmission rates, higher rates of discharge to home and lower 30-day post discharge Medicare costs.12-13
Strategies that help reduce hospital length of stay and improve discharge efficiency and ultimately reduce boarding in the emergency department. Emergency physicians know first-hand the advantages in communication and workflow as most of us work in designated zones and lead care teams dedicated to the patients placed in a particular geographic area.
When hospitalists consider the “geography” question, we can bring an understanding of the issue both in the inpatient and ED universes. Supporting geographic localization strategy helps improve inpatient throughput help create open inpatient beds. And open beds are the only solution to the problem of emergency department boarding!
DR. WELCH has been a practicing emergency physician for over thirty years. She has written numerous articles and three books on ED quality, safety, and efficiency. She is a consultant with Quality Matters Consulting, and her expertise is in ED operations.
DR. VASQUEZ is an Assistant Professor of Medicine at Emory University. of Operations for the Division of Hospitalist Medicine at Emory. He writes a Hospitalist Medicine Blog focused on operational excellence.
References
- Bryson C, Boynton G, Stepczynski A ,et al. Geographical assignment of hospitalists in an urban teaching hospital: feasibility and impact on efficiency and provider satisfaction. Hosp Pract (1995). 2017;45(4):135-142.
- Singh S, Tarima S, Rana V, et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551-556.
- Mirabella AC, McAmis NE, Kiassat C, et al. Preferences to improve rounding efficiency amongst hospitalist: a survey analysis. J Community Hosp Intern Med Perspect. 2021;11(4):501-506. Mirabella AC, McAmis NE, Kiassat C, et al. Preferences to improve rounding efficiency amongst hospitalist: a survey analysis. J Community Hosp Intern Med Perspect. 2021;11(4):501-506.
- Huang KTL, Minahan J, Brita-Rossi P, et al. All together now: impact of a regionalization and bedside rounding initiative on the efficiency and inclusiveness of clinical rounds. J Hosp Med. 2017;12(3):150-156.
- O’Leary KJ, Wayne DB, Landler MP, et al. Impact of localizing physicians to hospital units on nurse-physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223-1227.
- Williams A, DeMott C, Whicker S, et al. The impact of resident geographic rounding on rapid responses. J Gen Intern Med. 2019;34(7):1077-1078.
- Klein AJ, Veet C, Lu A, et al. The effect of geographic cohorting of inpatient teaching services on patient outcomes and resident experience [published online ahead of print January 24, 2022]. J Gen Intern Med.
- Singh S, Fletcher KE. A qualitative evaluation of geographical localization of hospitalists: how unintended consequences may impact quality. J Gen Intern Med. 2014;29(7):1009-1016.
- Coates E, Quisenberry E, Williams B, et al. Focusing hospitalist roles on either admitting or rounding facilitates unit-based assignment and is associated with improved discharge efficiency. Hosp Pract (1995). 2021;49(5):371-375.
- Ibrahim H, Harhara T, Athar S, Nair SC, Kamour AM. Multi-Disciplinary Discharge Coordination Team to Overcome Discharge Barriers and Address the Risk of Delayed Discharges. Risk Manag Healthc Policy. 2022 Feb 2;15:141-149.
- Wells M, Coates E, Williams B, et al. Restructuring hospitalist work schedules to improve care timeliness and efficiency. BMJ Open Qual. 2017;6(2):e000028.
- van Walraven C. The influence of hospitalist continuity on the likelihood of patient discharge in general medicine patients. J Hosp Med. 2018;13(10):692-694.
- Goodwin JS, Shuang Li, Yong-Fang K. Association of the work schedules of hospitalists with patient outcomes of hospitalization. JAMA Intern Med. 2020;180(2):215-222.
Pages: 1 2 3 | Single Page





No Responses to “The Hospital Geographic Zone Debate Pendulum Is Swinging Back”