
Approximately 35 million children in the United States visit emergency departments (EDs) each year.1 More than 80 percent of those ED visits occur in community hospitals that see fewer than 10 children daily.1
Explore This Issue
ACEP Now: February 2026 (Digital)Regardless of size, volume, or location, it is important that every ED in the United States is properly equipped to care for children. Despite this need, because of limited resources, many general EDs focus their attention mainly on infrastructure to support the care of adult patients, who constitute the bulk of their patient volumes. This leaves many EDs with significant gaps in the pediatric-specific equipment, resources, and clinical practice protocols needed to adequately respond to the needs of ill or injured children.
Studies have demonstrated that having a pediatric emergency care coordinator (PECC) to champion pediatric causes and address these gaps significantly improves pediatric readiness of EDs and that high pediatric readiness is associated with as much as 76 percent lower mortality risk.1,2 Yet only 29 percent of EDs have both the recommended physician and nurse PECC.1 To help support and grow PECCs, the Emergency Medical Services for Children Innovation and Improvement Center (EIIC) developed the Emergency Department PECC Module Series, a free, online educational resource designed for both new and existing physician and nurse PECCs.
What Is a PECC?
A PECC, also known as a pediatric champion, is an ED clinician (usually a nurse or physician) who helps ensure that systems, staff, and resources are in place to deliver high-quality emergency care for children. Research indicates that having both a physician and nurse PECC is among the most effective ways to improve pediatric readiness in an ED.1 The PECC role supports the seven key areas of pediatric readiness: coordination of care; policies, procedures, and protocols; care team competencies; quality improvement; patient safety; pediatric-specific equipment, supplies, and medications; and support services.
Why It Matters
Evidence shows that children with an acute medical condition who are treated in EDs with a higher pediatric readiness score (minimum of 88 on a 100-point scale) have a 76 percent lower mortality risk. Similarly, acutely injured children who are treated at a higher pediatric ready hospital have a 76 percent lower risk of death from their injuries.3 Nationally, this adds up to the potential saving of 2,000 pediatric lives in the U.S. each year,2 at a cost of only $4 to $48 per pediatric patient.4 The PECC Module Series helps hospitals move closer to full readiness by providing standardized, evidence-based guidance.5 It also supports hospitals seeking to meet National Pediatric Readiness Project (NPRP) benchmarks or develop a sustainable PECC program.
About the PECC Module Series
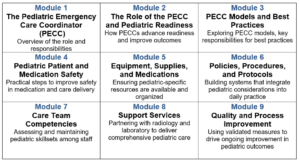
The nine-module series offers an overview of the PECC role, outlines best practices, and provides actionable strategies to enhance pediatric readiness in any ED. Each self-paced module takes less than 15 minutes to complete and includes a certificate of completion, ideal for nurses, physicians, advanced practice clinicians, administrators, and anyone involved in pediatric emergency care.
Implementation and Impact
The modules are flexible, accessible, and perfect for use during staff onboarding, annual competencies, or departmental training. By designating a physician and nurse PECC and completing the series, EDs can:
- Improve coordination of pediatric policies and training;
- Promote safe and consistent care for children;
- Strengthen interdisciplinary teamwork;
- Enhance quality improvement efforts and data tracking;
- Integrate pediatric considerations into disaster preparedness; and
- Ensure pediatric equipment, supplies, and medications are readily available.
Get Started
The ED PECC Module Series highlights a growing understanding that pediatric readiness is both achievable and essential in all EDs. As more hospitals adopt the PECC model and incorporate these educational tools into practice, the overall impact will be stronger systems, more confident teams, and better care for children in every community. This series can also help individual EDs to prepare for the next nationwide Pediatric Readiness Assessment, which begins in March 2026, providing a timely opportunity to evaluate and enhance their ED before the survey begins.
Learn more and access the modules here.
 Dr. Saidinejad is a professor of clinical emergency medicine and pediatrics at the David Geffen School of Medicine at UCLA, director of the Health Services and Outcomes Research Institute at the Lundquist Institute for Biomedical Innovation at Harbor UCLA, and director of pediatric research and scholarship, department of emergency medicine at the Harbor UCLA Medical Center.
Dr. Saidinejad is a professor of clinical emergency medicine and pediatrics at the David Geffen School of Medicine at UCLA, director of the Health Services and Outcomes Research Institute at the Lundquist Institute for Biomedical Innovation at Harbor UCLA, and director of pediatric research and scholarship, department of emergency medicine at the Harbor UCLA Medical Center.
 Ms. Goodman is project manager of the Knowledge Management Domain Emergency Medical Services for Children Innovation and Improvement Center at the Lundquist Institute for Biomedical Innovation at Harbor-UCLA.
Ms. Goodman is project manager of the Knowledge Management Domain Emergency Medical Services for Children Innovation and Improvement Center at the Lundquist Institute for Biomedical Innovation at Harbor-UCLA.
References
- Remick KE, Hewes HA, Ely M, et al. National Assessment of Pediatric Readiness of US Emergency Departments During the COVID-19 Pandemic.
- Newgard CD, Lin A, Malveau S, et al. Emergency Department Pediatric Readiness and Short-term and Long-term Mortality Among Children Receiving Emergency Care. JAMA Netw Open. 2023;6(1):e2250941.
- Ames SG, Davis BS, Marin JR, et al. Emergency Department Pediatric Readiness and Mortality in Critically Ill Children. Pediatrics. 2019;144(3):e20190568.
- Newgard CD, Lin A, Goldhaber-Fiebert JD, et al. State and National Estimates of the Cost of Emergency Department Pediatric Readiness and Lives Saved. JAMA Netw Open. 2024;7(11):e2442154.
- Remick KE, Gausche-Hill M, Lin A, et al. The hospital costs of high emergency department pediatric readiness. J Am Coll Emerg Physicians Open. 2024;5(3):e13179.




No Responses to “Strengthen Pediatric Emergency Care with New Free Modules”