
Three years ago I noticed I was not hearing well through my stethoscope. I decided to try an in-line analog amplifier that would work with my standard stethoscope. I was pleased with the result.
Explore This Issue
ACEP Now: Vol 39 – No 08 – August 2020Unfortunately, over time my hearing continued to deteriorate. I often asked patients and nurses to repeat themselves or speak loudly. I could hear people speak but not understand the words. People speaking behind me thought I was ignoring them. I needed to turn up the volume on the radio and TV, and I found hearing my cell phone challenging.
I made an appointment with an audiologist, and she performed an audiogram. The audiogram showed high-end hearing loss, and she recommended hearing aids. We talked about my work environment and stethoscope use and made a plan. I now wear behind-the-ear hearing aids with a fenestrated dome, which allows me to continue using my same amplified stethoscope. My hearing is greatly improved, and I rarely ask people to repeat themselves.
This approach worked for me, but everyone is different. Below, I discuss the various considerations and options in stethoscopes and hearing aids.
Keep in Mind
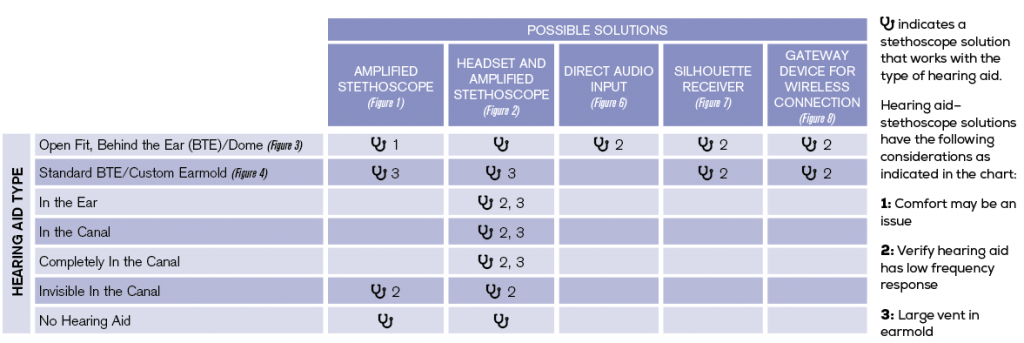
When thinking about stethoscope solutions, we first must understand that many heart, lung, and bowel sounds are low-frequency signals, and many current hearing aids don’t provide amplification of those frequencies. Therefore, it may not help you to send the stethoscope signal through certain hearing aids.
The good news: Most individuals with hearing loss retain hearing in the low frequencies. Those individuals can use open-fit hearing aids, which leave the ear canal largely open allowing low-frequency sounds to come in naturally. With such hearing aids, you can route the stethoscope signal past them.
Keep in mind that when an individual with normal hearing uses a stethoscope, their ears are blocked and their listening is focused on the stethoscope’s sounds. In contrast, when using a stethoscope with hearing aids, the hearing aid microphone remains on while you listen to the stethoscope. This may prove distracting because the sounds in the room will continue to be amplified through the hearing aids. If it is distracting, the audiologist can create a hearing aid program in which the microphones can be turned off at the hearing aid or remotely prior to using the stethoscope.
Last but not least, remember that if you do or will wear hearing aids, the goal is always to leave them in place. Removing and replacing hearing aids with each use of the stethoscope is not realistic.
The Options
No Hearing Aids: If you do not use hearing aids but know you aren’t hearing through your standard stethoscope as well as you used to, you can, like me, purchase an amplified stethoscope (see Figure 1). These are typically battery-operated, and you’ll want to become familiar with the on/off and volume up/down features.
Invisible Hearing Aids: If you use the tiny, invisible-in-the-canal hearing aids and they are seated deeply in your ear canals, you may be able to use a regular or amplified stethoscope if it is comfortable to put the stethoscope earpieces in your ears. If not, you’ll want to use a stethoscope connected to a headset that clamps over the ears (see Figure 2).

Figure 2: An amplified stethoscope with a headset.
Open Fit, Behind the Ear: Individuals with normal low-frequency hearing will often use open-fit, behind-the-ear hearing aids (see Figure 3). A small dome at the end of the tube fits in the ear, leaving the canal largely open. Depending on ear canal size and the placement of the dome in the ear canal, these hearing aid users may also be able to place an amplified stethoscope tip in the ear canal along with the dome. If this is not comfortable, use a stethoscope connected to a headset.

Figure 3 (LEFT): An open-fit behind-the-ear hearing aid.
Figure 4 (ABOVE): A standard behind-the-ear hearing aid with a custom earmold.
Figure 5 (ABOVE RIGHT): A special earmold that accepts a stethoscope tip.
Credit: David Baehren
In the Ear and Completely In the Canal: If these hearing aid users have some low-frequency hearing and wear open-fit hearing aids, they can also consider a stethoscope connected to a headset.
Behind the Ear with Earmold: If you use behind-the-ear hearing aids connected to a standard earmold (see Figure 4), have the audiologist remake the earmold to include a stethoscope vent. This is a large air hole in the earmold into which you can insert the stethoscope’s metal tip (see Figure 5). You’ll want to use an amplified stethoscope because it will go directly to the ear with hearing loss. An earmold with a large vent also can use a headset.
Direct Connections: Behind-the-ear hearing aids can be outfitted with a connector that will allow a cord to run directly from the stethoscope to the bottom of the hearing aid. This sends the stethoscope signal directly through the hearing aid’s signal processor (see Figure 6). The audiologist should verify the hearing aid can transmit the needed low frequencies.

Figure 6 (LEFT): Direct audio input from stethoscope to hearing aid.
Figure 7 (ABOVE): A hearing aid telecoil receiving an induction signal.
Figure 8 (RIGHT): A wireless stethoscope-to–hearing aid gateway device.
Credit: David Baehren
If your behind-the-ear hearing aid is equipped with a telecoil (ie, circuitry that picks up electromagnetic induction signals), you could plug a silhouette connection to the stethoscope (see Figure 7). The silhouettes are placed behind the hearing aids, and the signal is transmitted wirelessly. The listener must change the hearing aid program to the telecoil program setting. Again, the audiologist should verify the telecoil circuity can produce the needed low frequencies.
Wireless Connections: No stethoscopes transmit a Bluetooth signal directly to hearing aids. If a hearing aid user wants a wireless connection, a gateway device that can transit a signal to the hearing aid wirelessly from a digital stethoscope (see Figure 8) might do the trick. Again, the audiologist should verify the hearing aid can transmit the needed low frequencies. This solution can work for cochlear implant users as well.
Medical Students
The student with hearing loss who must learn to use a stethoscope is different from an experienced health care worker who gradually experiences hearing loss after practicing for years. A student does not know what they are listening for and may not be able to judge if they are hearing adequately. Such students should be encouraged to obtain an amplified stethoscope with a second listener port that an instructor can plug into and listen with the student. This will allow the instructor to judge whether the student is hearing adequately through the amplified stethoscope by asking the student to describe the signals they hear.
Final Thoughts
If your health care setting typically provides stethoscopes, the workplace should purchase an amplified stethoscope for you, too. If not, you will need to supply your own device.
Finally, if you haven’t yet purchased hearing aids, let the audiologist know you are a stethoscope user so the hearing aid recommendation can be at least partly based on ease of access to sounds through a stethoscope.
Dr. Baehren is an emergency physician in Ohio.





One Response to “Stethoscopes & Hearing Aids: Choosing the Right Devices for You”
June 28, 2021
rahul kumarWhere I can buy a amplified stethoscope..