Opioids have a place in the emergency department for the treatment of acute pain. However, they can also lead to significant morbidity and mortality with their misuse. The United States is in the middle of an epidemic, seeing an increasing number of preventable deaths and emergency department visits due to prescription opioid abuse. Of the more than 47,000 lethal opioid drug overdoses in the United States in 2014, 18,893 were related to prescription pain relievers, and 10,574 were related to heroin.1 According to the Centers for Disease Control and Prevention, 259 million prescriptions were written for opioids in 2012—enough for every U.S. adult to have their own bottle of pills.2
Explore This Issue
ACEP Now: Vol 35 – No 08 – August 2016After residency, I completed a yearlong emergency medicine acute pain management fellowship. My training included managing chronic pain with and without opioids, performing ultrasound-guided nerve blocks, and understanding best practice for acute pain control. My training extended to rotations with orthopedic spine surgery, neurology, radiology, physical medicine and rehabilitation, palliative care, and addiction medicine. During my fellowship year, I was exposed to the concept that for the majority of painful conditions, opioids are not immediately necessary but rather should be reserved as a last resort and only for severe pain. Physicians must be aware of the non-opioid modalities and medications available and work to integrate them into their day-to-day practice.
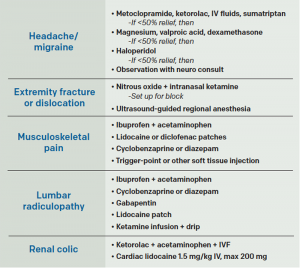
(click for larger image)
Table 1. Clinical Applications for ALTO Program Protocols
St. Joseph’s Regional Medical Center in Paterson, New Jersey, launched a formal program called Alternatives to Opiates (ALTO) to help improve pain management, patient care, and patient safety. The ALTO program utilizes targeted non-opioid medications, trigger-point injections, nitrous oxide, and ultrasound-guided nerve blocks to tailor patients’ pain management needs and avoid opioid use whenever possible.
Not every condition is appropriate for ALTO treatment. Cancer pain, significant trauma, or intra-abdominal pathology are conditions in which opioids are appropriate and often required. Examples of ALTO treatment include kidney stone pain now being treated with intravenous lidocaine instead of opioids; acute low back pain being treated with a combination of oral and topical pain medications, as well as trigger-point injections; extremity fractures being treated with focused ultrasound-guided nerve blocks; and acute headache and migraine pain being treated based on an algorithm using a variety of non-opioid medications. However, if patients’ pain is not adequately managed using ALTO techniques, opioids are used as second line.
Through the ALTO program, the emergency department is taking every step it can to decrease its opioid use in and out of the hospital. It has partnered with the St. Joseph’s Healthcare System Overdose Prevention and Naloxone Distribution Program to educate friends and family members of high-risk individuals about prescription opioid abuse and provide a naloxone kit to be kept in the home.
Additionally, the principles of the ALTO program have been adopted by the St. Joseph’s Departments of Family Medicine, Chronic Pain Management, PM&R, and Psychiatry. The multidisciplinary team works to tailor treatment plans for all patients. The ALTO program works closely with surrounding mental health facilities and detox centers such as Eva’s Village and the Straight & Narrow program. Peer screeners evaluate opioid-addicted patients in the emergency department in an effort to enroll them into a detox program immediately following their ED discharge.
Through education, implementation of novel concepts, and partnerships within the community, the ALTO program is changing the practice of pain management; the goal is to make the program a national model.
If you are interested in finding out more about the program or joining the newly formed ACEP Pain Management Section, please contact me or join the section.
Dr. LaPietra is the medical director of emergency medicine pain management at St. Joseph’s Regional Medical Center, Paterson, New Jersey, and chair of the ACEP Pain Management Section.
References
- Number and age-adjusted rates of drug-poisoning deaths involving opioid analgesics and heroin: United States, 2000–2014. Center for Disease Control and Prevention website. Accessed June 9, 2016.
- Opioid painkiller prescribing: where you live makes a difference. Centers for Disease Control and Prevention website. Accessed June 9, 2016.
Pages: 1 2 3 | Multi-Page





No Responses to “St. Joseph’s Regional Medical Center Aims to Avoid Opioid Use in Emergency Department”