The Case
A 50-year-old male with no known past medical history is brought to the emergency department by EMS after his wife found him down with right-sided flaccidity and aphasia. A prehospital stroke code was called in the field. Upon arrival, the patient is found to have no movement in the right upper or lower extremity, a left sided gaze, and complete aphasia. Computed tomography (CT) without contrast was performed and revealed a large left middle cerebral artery (MCA) thrombosis with infarct and bilateral subarachnoid hemorrhages. Tissue plasminogen activator (tPA) is not given due to subarachnoid hemorrhage. Neuro-intervention is consulted and brings the patient to the angiography suite to perform an endovascular thrombectomy extending from the terminus of the left internal carotid artery (ICA) to the left MCA. Following thrombectomy, the patient has good blood flow to left ICA and MCA.
Explore This Issue
ACEP Now: Vol 38 – No 08 – August 2019Slam-dunk stroke code with resolution of the cause?
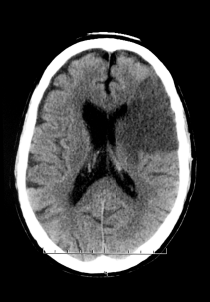
Axial nonenhanced CT of the head shows acute middle cerebral artery infarction.
Medical Body Scans/Science Source
History obtained from the wife shortly after the patient’s admission reveals that, over the previous six months, the patient had experienced intermittent fevers, night sweats, and a 25-pound weight loss. She adds that the patient recently emigrated from the Dominican Republic, where he had been evaluated for these symptoms, though he was never given a definitive diagnosis.
The patient subsequently receives a transesophageal echocardiogram, which reveals a bicuspid aortic valve with vegetations and mitral valve abscess. He is started on empiric antibiotics for endocarditis. Blood cultures grow Streptococcus mitis. The patient has a complicated recovery requiring percutaneous endoscopic gastrostomy tube placement, physical therapy, and daily intravenous antibiotics. Despite a complicated course over the period of a month, the patient has relative improvement in symptoms, begins to move his right upper and lower extremities, and regains his speech, but with dysphasia. He is discharged to a subacute rehabilitation facility with the diagnosis of a left MCA stroke secondary to septic embolus from infective endocarditis.
Causes of Stroke
Stroke is a common presentation to the emergency department. Most emergency physicians are well versed with the presentation and are trained to think stroke with thrombus means give tPA (controversy aside). However, the presumption of traditional ischemic stroke in all patients with stroke-like symptoms can result in disastrous consequences.
Ischemic strokes can be subdivided:
- Thrombotic
- Local obstruction of an artery that can be due to a variety of causes, most commonly atherosclerosis
- Most commonly occur in older patients
- Embolic
- Refers to a stroke that presents after an obstruction from particles or clot that originated in a different part of the body
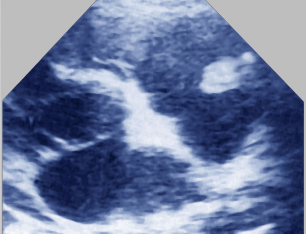
Cardiac ultrasound of infectious endocarditis. Note the vegetation in the trunk of the pulmonary artery.
James Cavallini
Clinically, both of these ischemic entities are treated similarly in the emergency department. If there is an occlusion and the patient has no signs of bleeding and falls into the appropriate time frame, tPA should be strongly considered. Depending on your institution, there should also be consultation with neurosurgery and neuro-intervention for potential thrombolysis, but that’s not the end of the evaluation.
Embolic stroke has multiple causes and can arise from the heart, aorta, or any large vessel. In this subset, we have the opportunity for further investigation and potential early intervention. Factors that suggest embolic stroke, triggering us to begin thinking of other causes, include:1
- Sudden and maximal onset of stroke symptoms
- Decreased level of consciousness
- Large vessel occlusion (anterior, middle, or posterior cerebral arteries, and the carotid, vertebral, or basilar arteries)
- Wernicke or global aphasia without hemiparesis
In a patient where embolic stroke is suspected, additional workup is warranted and may benefit the patient. A full set of vital signs (including a temperature), ECG, laboratory diagnostics, CT angiography of the brain extending from the aortic arch, a bedside echocardiogram or point-of-care ultrasound, and possible early cardiology consultation are essential components of the evaluation. Treatment decisions must be in concert with neurology colleagues.
- Common treatable causes of embolic stoke seen in the emergency department include:
- New-onset atrial fibrillation
- Recent myocardial infarction
- Infective endocarditis with septic emboli
- Carotid, vertebral, basilar, or aortic dissection
Along with true cerebrovascular accident, emergency physicians must be aware of the many potential stroke mimics. The list is not exhaustive, but some common mimics include hypoglycemia, Todd’s paralysis, migraines, malignancy, factitious disorder/malingering, and many others.2,3 Prior to heading down a typical stroke treatment algorithm, pause to consider these alternative diagnoses.
Discussion
Cerebrovascular accident is a commonly encountered and severely debilitating disease. As we protocolize early stroke management, diagnostic anchoring to “just” a stroke and lack of investigation into stroke mimics or secondary causes of stroke are real risks. Strokes that are embolic in nature can originate from a variety of causes, which will likely alter the overall approach and management of the patient. It is imperative that emergency physicians identify which patients may have an embolic stroke and investigate for reversible or treatable causes. Although not every stroke patient will have a source identified beyond traditional atherosclerotic disease, consideration of secondary causes has the potential to benefit our patients greatly. In short, all strokes are not created equal.
 Dr. Isenburg is an emergency medicine resident at St. Joseph’s University Medical Center in Paterson, New Jersey.
Dr. Isenburg is an emergency medicine resident at St. Joseph’s University Medical Center in Paterson, New Jersey.
 Dr. Boothe is an emergency and palliative care physician at St. Joseph’s University Medical Center.
Dr. Boothe is an emergency and palliative care physician at St. Joseph’s University Medical Center.
References
- Arboix A, Alio J. Acute cardioembolic cerebral infarction: answers to clinical questions. Curr Cardiol Rev. 2012;8(1):54-67.
- Merino JG, Luby M, Benson RT, et al. Predictors of acute stroke mimics in 8187 patients referred to a stroke service. J Stroke Cerebrovasc Dis. 2013;22(8):e397-e403.
- Tobin WO, Hentz JG, Bobrow BJ, et al. Identification of stroke mimics in the emergency department setting. J Brain Dis. 2009;1:19-22.
Pages: 1 2 3 | Multi-Page




No Responses to “Simple Ischemic Stroke: Is There Really Such a Thing?”