The Case
A 51-year-old male presents to the emergency department with a sudden-onset, severe, left-sided flank pain radiating to his groin. It began an hour before arrival. The pain was associated with nausea, vomiting, and difficulty urinating. He does not have a history of kidney stones and is currently writhing around on the stretcher.
Explore This Issue
ACEP Now: Vol 37 – No 05 – May 2018Background
About 1 to 5 percent of the U.S. population suffers from kidney stones.1 The typical ED presentation is sudden onset of pain radiating from the flank to lower abdomen accompanied by nausea, vomiting, and microscopic hematuria.2
Renal colic is very painful condition. Opioids are often used for pain relief, along with intravenous nonsteroidal anti-inflammatory drugs. Alpha blockers have been repeatedly studied for use with renal colic. An excellent randomized controlled trial, published in Annals of Emergency Medicine, showed no significant difference in stone passage or time to stone passage with tamsulosin compared with placebo in calculi <10mm.3
Lidocaine may be a useful alternative, as it has been used to effectively treat visceral and neuropathic pain.4 Finding non-opioid alternatives to treat painful conditions is timely given the heightened attention on the opioid epidemic.
Clinical Question
In patients presenting to the emergency department with renal colic, is IV lidocaine as or more effective than IV opioids for pain control?
Reference
Soleimanpour H, Hassanzadeh K, Vaezi H, et al. Effectiveness of intravenous lidocaine versus intravenous morphine for patients with renal colic in the emergency department. BMC Urol. 2012;12:13.
- Population: Adults 18–65 years of age presenting to the emergency department with abdominal pain suggesting renal colic and hematuria on urine analysis.
- Excluded: Pregnancy; allergy to lidocaine or morphine; or history of renal, hepatic, or cardiac disease.
- Intervention: IV lidocaine 1.5 mg/kg (max of 200 mg).
- Comparison: IV morphine 0.1 mg/kg (max of 10 mg).
- Outcome: Pain on visual analog scale (VAS) at 5, 10, 15, and 30 minutes post intervention.
Authors’ Conclusions
“Changing the smooth muscle tone and reducing the transmission of afferent sensory pathways, lidocaine causes a significant reduction in pain.”
Key Results
The researchers enrolled 240 patients into the study, with 120 in each group. The mean age was in the mid 30s.
The trial was considered “accomplished” when either the patient had a pain score of less than 3 for 30 minutes after the last analgesic dose, or the 10 mL of solution in the syringe (either 200 mg lidocaine or 10 mg morphine) was exhausted. See Table 1 for the results.
- 90 percent (108/120) of patients responded to lidocaine successfully.
- 70 percent (84/120) of patients responded to morphine successfully.
- The number of patients experiencing side effects was similar in both groups.
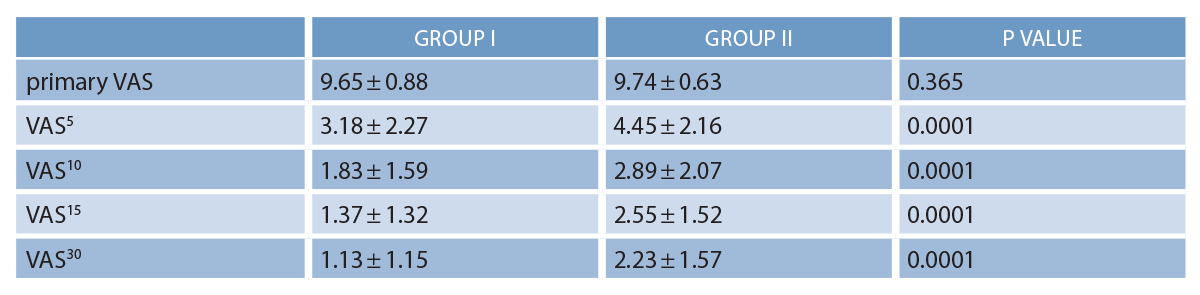
(click for larger image) Table 1: Comparison of the Mean Value of Pain Reduction Between Two Groups
Source: Soleimanpour H, et al. BMC Urol. 2012; 12:13. Creative Commons Attribution License.
Evidence-Based Medicine Commentary
- Renal Colic: I am unsure if the patients enrolled in this trial had renal colic. Inclusion was based on history and hematuria. Follow-up studies included a kidney-ureter-bladder X-ray and/or sonography. Neither of these diagnostic modalities are gold standard methods for diagnosing nephrolithiasis. This could have introduced diagnostic bias into the study.
- Consecutive Patients: The authors did not explicitly state they used consecutive recruitment, only that they used Randomization.com as their randomization tool. A lack of consecutive recruitment can lead to selection bias.
- Patient Blinding: It is possible that participants were aware of their group allocation. This is because morphine can produce side effects that could have unmasked the blinding. It is unclear if this potential bias would favor the morphine or the lidocaine group.
- Provider Blinding: The providers may have also been unblinded, which could introduce bias into the trial. This is because differences in weight-based dosing would result in different volume administrations of medications (ie, a 100 kg patient would be dosed 150 mg [7.5 mL] of lidocaine but would be dosed 10 mg [the full 10 mL] of morphine).
- Clinical Versus Statistical Significance: This is the key limitation of the trial. Although the results obtained statistical significance, the standard deviations of the means in every group at each measured time interval overlap and do not appear to have clinical significance.
Bottom Line
This study does not provide good evidence for using lidocaine to treat patients presenting to the emergency department with renal colic.
Case Resolution
You perform a bedside ultrasound, and it demonstrates mild left hydronephrosis. The patient is given ketorolac 10 mg IV and his pain resolves. He is then discharged home with analgesics, expectant management, and explicit instructions on when to return to the emergency department.
Thank you to Tony Seupaul, MD, chairman of the department of emergency medicine at the University of Arkansas at Little Rock, and Rachel Littlefield, MD, who is an emergency medicine resident at the University of Arkansas, for their help with this review.
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.
References
- O’Connor A, Schug SA, Cardwell H. A comparison of the efficacy and safety of morphine and pethidine as analgesia for suspected renal colic in the emergency setting. J Accid Emerg Med. 2000;17(4):261-264.
- Dave C, Faraj K, Shetty S. Nephrolithiasis. Medscape web site. 2017. Accessed April 12, 2018.
- Furyk JS, Chu K, Banks C, et al. Distal ureteric stones and tamsulosin: a double-blind, placebo-controlled, randomized, multicenter trial. Ann Emerg Med. 2016;67(1):86-95.e2.
- Ferrini RA, Paice JA. How to initiate and monitor infusional lidocaine for severe and/or neuropathic pain. J Supportive Oncol. 2004, 2:90-94.
Pages: 1 2 | Multi-Page





One Response to “Should You Use Lidocaine Instead of Opioids to Treat Renal Colic?”
May 27, 2018
Mark Mosley MDThis is only an important question to ask if you believe that giving opioids to a low risk opioid naive patient with objective symptoms somehow increases the odds of chronic opioid use or misuse.
The post-op surgical literature on opioid naive patients that does NOT screen out high risk patients (mental illness, smoking, alcohol, etc) finds that chronic use from opioid administration is 0.2 percent (close to zero).
So if you have a low risk patient with a kidney stone, give the poor soul whatever it takes to quickly, effectively, and safely make them better (this will likely include opioids in many real deal stones).
If you have a patient at high risk for opioid misuse (chronic pain, addiction including nicotine, psychiatric disease including depression and anxiety, or electronic pharmacy records indicating excessive scripts, then we should be comparing non-opioid medications (toradol versus lidocaine).
Not sure why the opioid crisis has put all of our patients into a one-size-fits-all category of always starting with a non-opioid approach?