
Give More to Get More
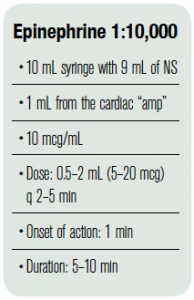
Time to paralysis is inversely proportional to cardiac output. Therefore, as the cardiac output decreases in hemodynamically unstable patients, time to full muscle relaxation is increased. To overcome this barrier, the dose of paralytics should be increased. Succinylcholine doses can be increased to 2 mg/kg and rocuronium to 1.6 mg/kg. In addition, medications that augment cardiac output can be beneficial here as well. The medication of choice is push-dose epinephrine. Given in 5–20 mcg bolus doses, it can augment both the patients’ blood pressure and cardiac output (see Table 1). For this reason, epinephrine is superior to phenylephrine for the purpose of intubating hemodynamically unstable patients. In such patients, phenylephrine may decrease cardiac output because it only offers vasoconstrictive effects, which may actually increase the length of time to paralysis.
Do You Have a Minute to Talk About Scopolamine?
If hemodynamically unstable patients need to be intubated but you only have a few minutes to prepare, consider pretreatment with scopolamine. By giving 0.4 mg of scopolamine a few minutes prior to induction, multiple advantageous effects can be achieved. Primarily, scopolamine acts as an amnestic agent, rendering patients memory-free if induction turns out to be inadequate. The side effect of scopolamine, tachycardia, can augment cardiac output as well.
Optimize Prime
There are other steps that can be taken besides medication choices to maximize patients’ chance of survival. Resuscitation fluids, whether blood products for trauma or crystalloid for hypovolemia, should be started prior to the intubation. Don’t wait until the induction agent has been given before volume resuscitating patients. Blood pressure goals for pre-intubated patients should be slightly higher than usual. Systolic blood pressure of 140 or mean arterial pressure of 80 for septic patients is ideal, knowing that the intubation itself will cause some degree of blood pressure reduction. To achieve this effect, start an inopressor (eg, push-dose epinephrine) prior to the intubation, along with the fluids that should already be infusing. For hemorrhaging trauma patients, while permissive hypotension is the goal, allowing the pressure to meander higher prior to placement of the endotracheal tube is ideal.
Low and Slow
Once patients are successfully intubated on the vent, what should the settings be to prevent further hypotension from the initiation of PPV? For most patients, a low peep and low tidal volume strategy of 6 cc/kg IBW should be enacted. This will minimize the degree to which venous return and preload are negatively affected. While these settings may place patients at risk for some degree of hypercarbia, such a result is acceptable provided patients are not suffering increase intracranial pressure or other cerebral insult.
Conclusion
Intubating hypotensive patients or patients who have the potential to become hypotensive is a procedure fraught with many pitfalls and possible missteps. Careful preparation and consideration of what harm the provider can conceivably cause can diminish these risks. As previously stated, hypotension during the intubation period has been shown to be an independent risk factor for mortality, therefore it is of utmost importance to take all imaginable measures to reduce its occurrence.
Pages: 1 2 3 | Single Page





One Response to “How To Prevent Peri-intubation Deaths with Careful Medication Choice”
May 24, 2014
jschaff112@gmail.comWhere is the mention of Rocuronium and Versed combo. I have used this or Vecuronium exclusively for many years without any incident. I have seen PLENTY of hypotension from Etomidate, the latest and greatest coming out of residency programs. And I routinely see the adrenergic state dissipate once the patient is paralyzed. A double whammy with Etomidate. I bet it is very useful for procedural sedation, just not for me.
And Sux is an old standard, but it has caveats in trauma and intracranial conditions where increased ICP occurs. Not my best choice again when the others are lacking in these adverse events and are just as useful or easy to use.