The role of emergency department physicians and leaders has been made dramatically more important due to the surges in demand and medical system challenges produced by the COVID-19 pandemic. However, it will be essential for those leaders to look at the trends present prior to the pandemic and to accurately predict how they will influence the patient populations of 2021 and beyond.
Explore This Issue
ACEP Now: Vol 39 – No 11 – November 2020The performance of emergency departments in 2019 has been summarized for the many members of the Emergency Department Benchmarking Alliance (EDBA), who provided the data needed to characterize operations prior to the pandemic. Many trends will continue, and some will be accelerated by the pandemic. Regardless, these trends all suggest emergency departments will see higher-acuity patients with more complex medical needs and play a crucial role in determining capacity. Most communities are aware of the emergency department as the portal for critical patients and unexpected events, but now the value in public health and managing community surges is even more visible—and maybe even more appreciated!
The results of the 2019 EDBA performance measures survey say emergency departments are seeing higher-acuity patients, more adults, and more EMS patients; are making more use of diagnostic tests; are transferring more ED patients; and are absorbing the early time of patients who need inpatient services (ie, boarding). The management expertise and dedication of ED leaders are therefore ever more necessary.
Here are four results lifted from the survey:
1) Fewer children are presenting to community emergency departments.
ED visits by patients under age 18 have decreased from about 22 percent in the years before 2011 to about 15 percent in 2019 (see Figure 1).
2) More patients are being transferred.
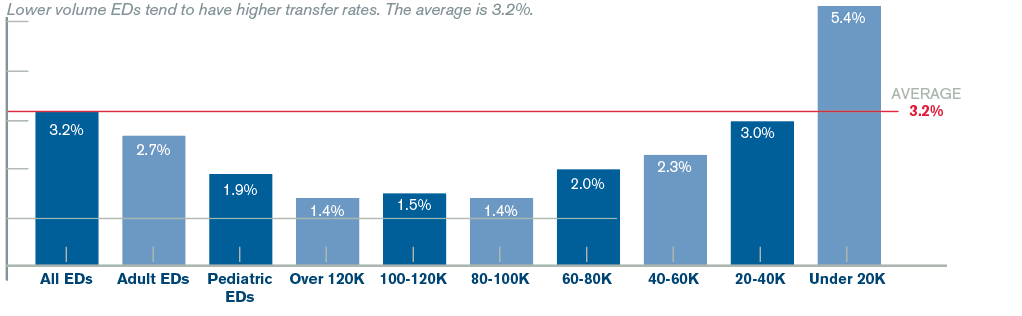
There are significant differences in rates of transfer to another hospital based on the features of emergency departments in the United States. The transfer rate is highest in small-volume emergency departments, which now amounts to 5.4 percent of the patients seen in those facilities. It appears fewer hospitals in rural communities have the resources to keep complex patients. They are closing service lines and have been unsuccessful in recruiting doctors willing to care for complex patients. Rural facilities also may incur financial penalties related to the inability to manage patients as expeditiously as larger hospitals.
ED transfer rates by cohorts (type of facility) are reflected in Figure 2. Transfer rates prior to 2011 were about 1.6 percent, and they have now doubled to 3.2 percent.
These numbers are primarily driven by smaller hospitals, but all types of emergency departments are trending toward more patient transfers. Of note, these data do not include freestanding emergency departments, which can place additional burdens on the transfer resources of hospitals and hospital systems.
3) The percentage of patients admitted from the emergency department to the hospital has rapidly increased.
About 67 percent of hospital admissions are processed through the emergency department. These admissions include patients seen in the emergency department and then placed in any inpatient area of the hospital, either as “full admission” or “observation status.” High-volume and adult-serving emergency departments tend to have high admission rates.
The average has increased from prior years to 22 percent (see Figure 3).
4) Patients who require ED boarding challenge ED operations.
Boarding time is an important contributor to overall patient processing, and it has remained stubbornly high, an annual average of about 115 minutes between 2012 and 2019.
ED boarding, time from decision-to-admit until the patient physically leaves the emergency department, remains a burden on ED performance. It accounts for about 38 percent of the time admitted patients spend in the emergency department. This time interval has been part of each hospital’s required data submission to the Centers for Medicare & Medicaid Services since 2013, and results are posted on the Hospital Compare website (www.medicare.gov/hospitalcompare). It was hoped that public posting of boarding would motivate hospital administrators to improve this metric. Unfortunately, despite the work of many ED and hospital leaders to reduce boarding time, the data for 2019 list the average interval at 118 minutes.
The EDBA Performance Measures Summits have been used to unify the definitions used across the industry, and that process has been used to accurately define boarding time and the burden on the emergency department of admitted patients. There is ongoing work to identify hospitals that have reduced boarding time by making ED patient flow more efficient.
Prioritizing ED Management Challenges
The need for emergency physicians has dramatically increased due to patient needs and medical system challenges fueled by the COVID-19 pandemic. However, the advent of telemedicine programs has provided another ready source of care for patients with low-acuity, unscheduled care needs; those patients will largely disappear from the ED population for the foreseeable future.
Emergency physician leaders must appreciate trends present through 2019 and work collaboratively with hospital leaders to serve a changing emergency population in 2021 and beyond. The need to move admitted patients up to the inpatient units is a particularly important management priority.
The EDBA Summits have provided a dedicated group of federal, regional, and emergency leaders the opportunity to develop reasonable standards and performance measures for the industry. The definitions published after the 2018 summit have recently been published, and they provide guidance to ED leaders who are developing data management processes that improve performance.1
Reference
- Yiadom MYAB, Napoli A, Granovsky M, et al. Managing and measuring emergency department care: results of the fourth Emergency Department Benchmarking Definitions Summit. Acad Emerg Med. 2020;27(7):600-611.
Pages: 1 2 3 | Multi-Page








No Responses to “Pre-COVID ED Trends Suggest More Challenges Lie Ahead”