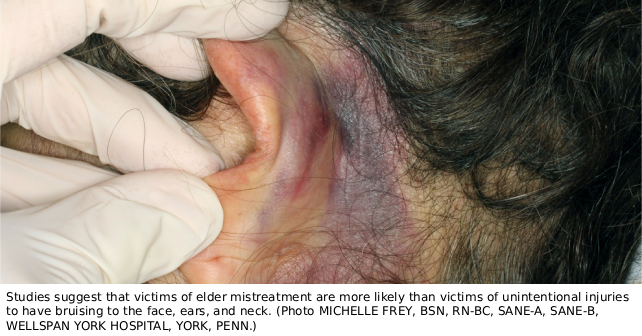
An 84-year-old woman is brought to the emergency department by her daughter for bruising to the left ear. The patient’s daughter states that she noted this injury when she picked her mother up at her brother’s house, where the patient usually resides. The patient has a history of dementia and cannot recall how the injury occurred.
Explore This Issue
ACEP Now: November 2025Introduction
The Centers for Disease Control and Prevention defines five types of elder abuse:1
- Physical abuse is illness, injury, functional impairment, or death resulting from the intentional use of physical force. Examples include hitting, kicking, or pushing.
- Sexual abuse is forced or unwanted sexual interaction. Examples include unwanted sexual contact or penetration or non-contact acts, such as sexual harassment.
- Emotional or psychological abuse refers to verbal or nonverbal behaviors that inflict anguish, fear, or distress. Examples include humiliation, threats, or harassment.
- Neglect is the failure to meet an older adult’s basic needs. These needs include food, water, shelter, clothing, hygiene, and essential medical care.
- Financial abuse is the illegal, unauthorized, or improper use of money, benefits, property, or assets for the benefit of someone other than the older adult.
It is difficult to determine the prevalence of elder abuse. In one study, it was found that one in 10 elders were victims of elder mistreatment.2 It is estimated that for every one case of elder abuse, neglect, exploitation, or self-neglect reported to authorities, about five more go unreported.3 A study in New York found that for every case made known to programs and agencies, 24 were not reported.4 Although physical abuse is less common than psychological abuse or neglect, victims of physical abuse are more likely to present to emergency departments or urgent care facilities. Emergency physicians are in a unique position to recognize and intervene in cases of elder mistreatment.
Patterns of Injury
To identify nonaccidental trauma (NAT) in elderly patients, emergency physicians must recognize the patterns of injury that are more common in cases of NAT than in accidental injury. This can be difficult due to normal physiologic changes of aging. There are, however, some red flags suggesting NAT. They include:
- Injuries inconsistent with reported mechanism or history;
- Delay in presentation;
- Multiple injuries at different stages of healing; and
- Specific patterns of injury more consistent with NAT than with accidental trauma.
Although research regarding patterns of injury in elder mistreatment isstill scarce, several studies have suggested that certain patterns of bruising are more common in NAT than in accidental trauma. Larger bruises (those greater than 5 cm in size) are more likely to be the result of abusive trauma.5 Victims of elder mistreatment are more likely than victims of unintentional injuries to have bruising to the face, ears, and neck. They are more likely to have injuries to the upper extremities and the torso, particularly the back.5,6,7 Injuries to the lateral and anterior upper arms are also common.8 Patterned injuries (wounds that reproduce the distinctive shape, size, or characteristics of the objects that caused them) are also more common in NAT.
Elderly victims of NAT are less likely to have fractures than victims of accidental trauma.6 However, research has indicated that certain types of fractures are more likely to occur in victims of NAT. Skull, face, and rib fractures are more often a result of NAT than of falls. Victims of elder abuse are also more likely to have multiple fractures.9
Reporting
Reporting requirements for elder abuse vary among jurisdictions. In most states, Adult Protective Services receives and investigates reports of elder abuse and neglect. It is important to know the reporting requirements and procedures for the jurisdictions in which you practice. Hospital social workers or clinical forensic examiners may be able to assist with reporting.
Case Conclusion
On further examination, the patient is found to have bruising on her back. A CT scan of the head does not show any acute traumatic injury. Given your concern for nonaccidental injury, you consult the forensic examiner’s team for assistance. Photos are taken for the medical record, and the case is reported to Adult Protective Services. The patient is discharged in the care of her daughter pending an investigation.
 Dr. Rozzi is an emergency physician, medical director of the Forensic Examiner Team at WellSpan York Hospital in York, Pennsylvania, and secretary of ACEP’s Forensic Section.
Dr. Rozzi is an emergency physician, medical director of the Forensic Examiner Team at WellSpan York Hospital in York, Pennsylvania, and secretary of ACEP’s Forensic Section.
 Dr. Riviello is chair of emergency medicine at Crozer-Keystone Health System and medical director of the Philadelphia Sexual Assault Response Center.
Dr. Riviello is chair of emergency medicine at Crozer-Keystone Health System and medical director of the Philadelphia Sexual Assault Response Center.
References
- Centers for Disease Control and Prevention. About Abuse of Older Persons. 2025. https://www.cdc.gov/elder-abuse/about/index.html. Accessed September 11, 2025.
- Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and Correlates of Emotional, Physical, Sexual, and Financial Abuse and Potential Neglect in the United States: The National Elder Mistreatment Study. Am J Public Health 2010;Feb;100(2):292-297.
- Acierno R, Hernandez-Tejada M, Muzzy W, Steve K. The National Elder Mistreatment Study. U.S. Department of Justice. 2009. Document 226456. https://www.ojp.gov/pdffiles1/nij/grants/226456.pdf.
- Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University and the New York City Department for the Aging. 2011. Under the Radar: New York State Elder Abuse Prevalence Study. https://ocfs.ny.gov/reports/aps/Under-the-Radar-2011May12.pdf.
- Wiglesworth, A, Austin, R, Corona, M, et al. Bruising as a Marker of Physical Elder Abuse. J Am Geriatr Soci 2009;57:1191-1196.
- Rosen T, LoFaso VM, Bloemen EM, et al. Identifying Injury Patterns Associated With Physical Elder Abuse: Analysis of Legally Adjudicated Cases. Ann Emerg Med 2020; 76(3):266-276.
- van Houten ME, Vloet LCM, Pelgrim T, et al. Types, characteristics and anatomic location of physical signs in elder abuse: A systematic review: Awareness and recognition of injury patterns. Eur Geriatr Med 2022;13(1):53-85.
- Ziminski, CE, Wiglesworth, A, Austin, R, et al. Injury patterns and causal mechanisms of bruising in physical elder abuse. JForensic Nurs 2013; 9(2):84-91.
- Gardezi M, Moore HG, Rubin LE, Grauer JN. Predictors of Physical Abuse in Elder Patients with Fracture. J Am Acad Orthop Surg Glob Res Rev 2022; 12;6(7):e22.00144.
Pages: 1 2 3 | Multi-Page





No Responses to “Patterns of Injury in Elder Abuse”