The Case
A 52-year-old male with a history of dyslipidemia presents to the emergency department after sustaining an injury to his left (nondominant) shoulder after colliding with another player during a soccer game. On examination, there is a loss of the normal rounded appearance of the shoulder. You suspect the patient may have a shoulder dislocation. He has no history of shoulder dislocations.
Explore This Issue
ACEP Now: Vol 39 – No 05 – May 2020Background
Shoulder dislocations are common in the emergency department. Emergency physicians frequently perform pre- and post-reduction X-rays for these patients. Some previous studies question whether these X-rays are necessary, especially in patients without direct trauma and a history of recurrent dislocations.1,2
Point-of-care ultrasound (POCUS) has been shown in previous studies to be sensitive and specific for diagnosing shoulder dislocations.3,4 This application can potentially reduce radiation exposure, cost, and time to diagnosis. However, prior studies on the use of POCUS for shoulder dislocations have used a variety of scanning techniques, and some have utilized as few as two sonographers.4
Clinical Question
Should you use POCUS to diagnose shoulder dislocations instead of an X-ray?
Reference: Secko MA, Reardon L, Gottlieb M, et al. Musculoskeletal ultrasonography to diagnose dislocated shoulders: a prospective cohort. Ann Emerg Med. 2020;S0196-0644(20)30008-1.
- Population: Adults with suspected shoulder dislocations.
- Exclusion: Patients with multiple traumatic injuries, decreased level of consciousness, or hemodynamic instability.
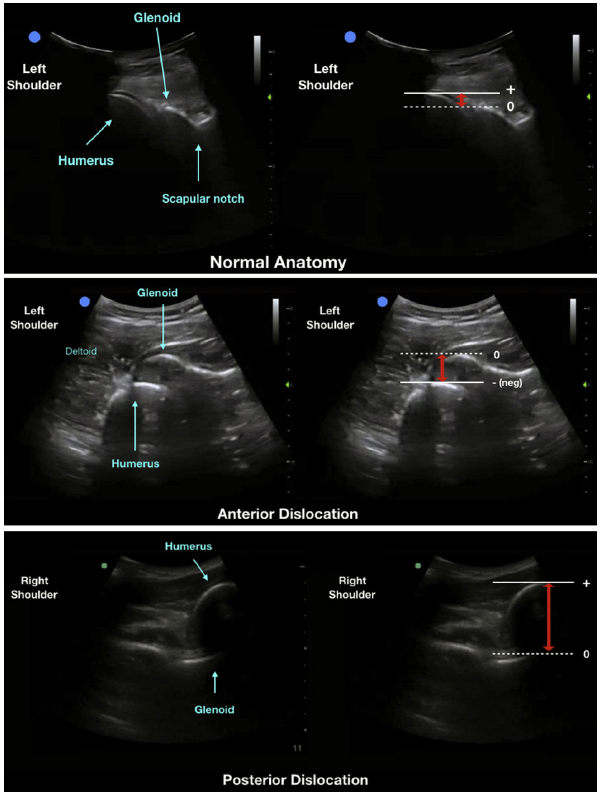
- Intervention: Pre- and post-reduction POCUS utilizing a posterior approach in which the probe traces along the scapular spine toward the glenohumeral joint (see original article for details).
- Comparison: X-rays pre- and post-reduction.
- Outcomes:
- Primary Outcome: Diagnostic accuracy of POCUS for shoulder dislocations.
- Secondary Outcomes: Presence or absence of fracture, time from triage to POCUS exam compared to X-ray, time from POCUS exam initiation to diagnosis, determination of glenohumeral distance of nondislocated and dislocated shoulders, and sonographer confidence in diagnosis.
Authors’ Conclusions
“A posterior approach point-of-care ultrasonographic study is a quick and accurate tool to diagnose dislocated shoulders. Ultrasonography was also able to accurately identify humeral fractures and significantly reduce the time to diagnosis from triage compared with standard radiography.”
Ann Emerg Med. 2020 Feb 25. doi: 10.1016/j.annemergmed.2020.01.008. © ACEP
Ultrasonographic images of the shoulder girdle, using a curvilinear probe demonstrating the normal anatomy of the left glenohumeral joint (A), a left anterior dislocation of the shoulder with humeral head displaced anterior to the glenoid (B), and a right posterior shoulder dislocation with the humerus displaced posterior to the glenoid (C). The adjacent images correspond to the measurement of the glenohumeral distance, indicated by the red arrows.
Key Results
The study enrolled 65 patients with a median age of 40 years. Fifty-eight percent were male, 49 percent had a dislocation (one inferior, two posterior, and 29 anterior), and 32 percent had a previous dislocation.
- Primary Outcome: Diagnostic accuracy.
- Sensitivity, specificity, positive predictive value, and negative predictive value were all 100 percent (95% CI, 87–100).
- Secondary Outcomes:
- 25/65 (38 percent) had fractures, with 13 Hill-Sachs/Bankart.
- Non–Hill-Sachs/Bankart fracture: Sensitivity 92 percent (95% CI, 60–99.6), specificity 100 percent (95% CI, 92–100), positive predictive value 100 percent (95% CI, 68–100), and negative predictive value 98 percent (95% CI, 89–99.9).
- POCUS was 43 minutes faster from exam to diagnosis compared to X-ray.
- The median glenohumeral distance was –1.83 cm (interquartile range [IQR] –1.98 to –1.41 cm) in anterior dislocations, 0.22 cm (IQR 0.10–0.35 cm) on nondislocated shoulders, and 3.30 cm (IQR 2.59– 4.00 cm) in posterior dislocations.
- Sonographers’ confidence in their POCUS diagnosis was 9.1 of 10 in nondislocated cases and 9.4 of 10 in dislocated cases.
Evidence-Based Medicine Commentary
- Convenience Sample: The study did not recruit consecutive patients but rather a convenience sample when one of six sonographers were available. There is a potential for selection bias with this type of sampling.
- Missing Data: All 32 patients with dislocations were supposed to have had a post-reduction POCUS performed. However, in five cases, this did not happen. The manuscript says it was because the study sonographer was unavailable after the reduction for various reasons without further explanation. This could have introduced some bias and increases our skepticism of the results.
- Missed Fractures: Twenty-five of 65 patients had fractures (38 percent). POCUS identified only 52 percent of those fractures. However, all but one of the missed fractures was a Hill-Sachs deformity or a Bankart lesion. Hill-Sachs and Bankart fractures are generally not relevant to the emergency management of patients with shoulder dislocations. POCUS was 92 percent sensitive (95% CI, 60–99.6%) and 100 percent specific (95% CI, 92–100%) for non–Hill-Sachs/Bankart fractures. This miss rate of 8 percent of non–Hill-Sachs/Bankart fractures is too high for American medicine.
- External Validity: Although the study was technically multicenter because two facilities were involved, one of the two sites enrolled only five patients. In addition, ultrasound fellows or ultrasound fellowship-trained attendings performed the scans. This makes us question the external validity of the study. If the ultrasounds were performed by typical community emergency physicians, we are unsure the same impressive results would be achieved.
- Time Saved: The median time to POCUS from triage was 51 minutes (IQR 36–77) compared to 101 minutes (IQR 73–134) for X-ray. The amount of time saved in the real world would depend on the system in which the physician is working. In a facility with single-physician coverage, the X-ray tech may complete the X-ray before the physician has an opportunity to perform an ultrasound. Last, they did not provide information on total ED length of stay.
Bottom Line
X-rays should continue to be the primary imaging modality of choice for most patients with suspected shoulder dislocations.
Case Resolution
The patient suffered direct trauma to the shoulder during a soccer game, which increased the probability of having a fracture dislocation of the shoulder. An X-ray is obtained and demonstrates an anterior dislocation. The Cunningham technique is used successfully, and the patient is discharged home with appropriate advice and follow-up.
Thank you to Dr. Tony Zitek, research director for the emergency medicine residency program at Kendall Regional Medical Center in Miami, for his help with this review.
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.
References
- Émond M, Gariepy C, Boucher V, et al. Selective prereduction radiography in anterior shoulder dislocation: the Fresno-Quebec rule. J Emerg Med. 2018;55(2):218-225.
- Harvey RA, Trabulsy ME, Roe L. Are postreduction anteroposterior and scapular Y views useful in anterior shoulder dislocations? Am J Emerg Med. 1992;10(2):149-151.
- Gottlieb M, Holladay D, Peksa GD. Point-of-care ultrasound for the diagnosis of shoulder dislocation: a systematic review and meta-analysis. Am J Emerg Med. 2019;37(4):757-761.
- Abbasi S, Molaie H, Hafezimoghadam P, et al. Diagnostic accuracy of ultrasonographic examination in the management of shoulder dislocation in the emergency department. Ann Emerg Med. 2013;62(2):170-175.
Pages: 1 2 3 | Multi-Page






No Responses to “New Study Compares POCUS with X-Ray for Shoulder Dislocations”