
The Case
A 62-year-old female with a history of anemia and hypertension presents following an episode of syncope that morning while making her coffee. She felt light-headed. As she reached for the wall, the room “went dark.” The next thing she remembers is waking up on the floor. She denies headache, chest pain, shortness of breath, or palpitations. She has been feeling well recently and eating and drinking
Explore This Issue
ACEP Now: Vol 38 – No 12 – December 2019as usual. She has been taking her antihypertensives as prescribed. She is now back to her neurological baseline but feels fatigued.
In the emergency department, she appears tired but well. Her vital signs and physical exam are unremarkable. She has no signs of head trauma, no cardiac murmurs, and no signs of heart failure. Her initial ECG is normal. Bloodwork has been sent to the lab. What is the utility of cardiac biomarkers in this patient? What will her ultimate ED disposition be if her workup is unremarkable?
The Tricky Problem of Syncope
In many ways, syncope management is a microcosm of emergency medicine. The differential diagnosis is broad, and the etiology is typically benign but rarely can also be serious or life-threatening. Safe medical decision-making requires a mixture of diagnostic acumen and risk stratification. Which patients can be safely discharged from the emergency department? Which require a stay in the observation unit or hospital? This question has vexed emergency clinicians for years.
Over the last 20 years, researchers have attempted to identify risk factors for adverse events after syncope. The usual suspects emerged: advanced age, history of heart disease, abnormal vital signs, abnormal ECG.
More recently, researchers have attempted to create simple, objective risk scores to help clinicians deliver sensible care to syncope patients—care that matches their risk profile.
The San Francisco Syncope Rule gained early acceptance but has gradually faded away after attempts to validate the score were unsuccessful.
Developing a New Metric
We wanted to know if we could improve clinical outcomes and reduce low-yield admissions by developing a more accurate and reliable syncope risk score. So with funding from the National Institutes of Health, we conducted a five-year multicenter study to enroll a large enough sample size. We included patients ages 60 years and older with an ED complaint of syncope or near syncope. We excluded patients with other causes of loss of consciousness (eg, concussion, hypoglycemia, seizure) and those with a serious diagnosis identified in the emergency department (eg, myocardial infarction, pulmonary embolism, gastrointestinal bleed).
After six years of hard work, and with the help of about a dozen collaborators, our syncope risk score, the aptly named “FAINT Score, was finally published in the Annals of Emergency Medicine.”1 In the end, we had enrolled more than 3,100 older adults with unexplained syncope or near syncope across 11 emergency departments in the United States. The primary outcome was death or serious cardiac event at 30 days.
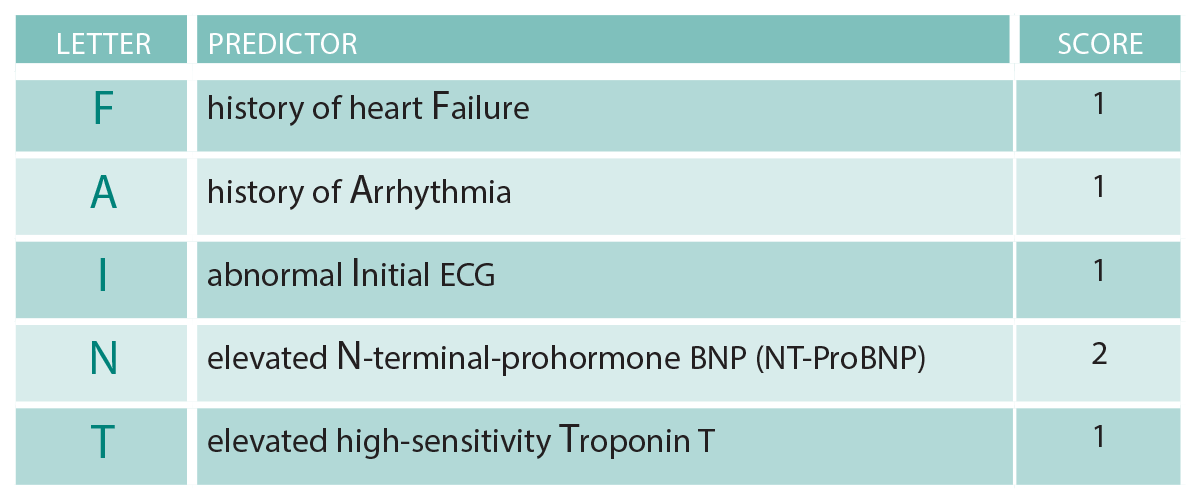
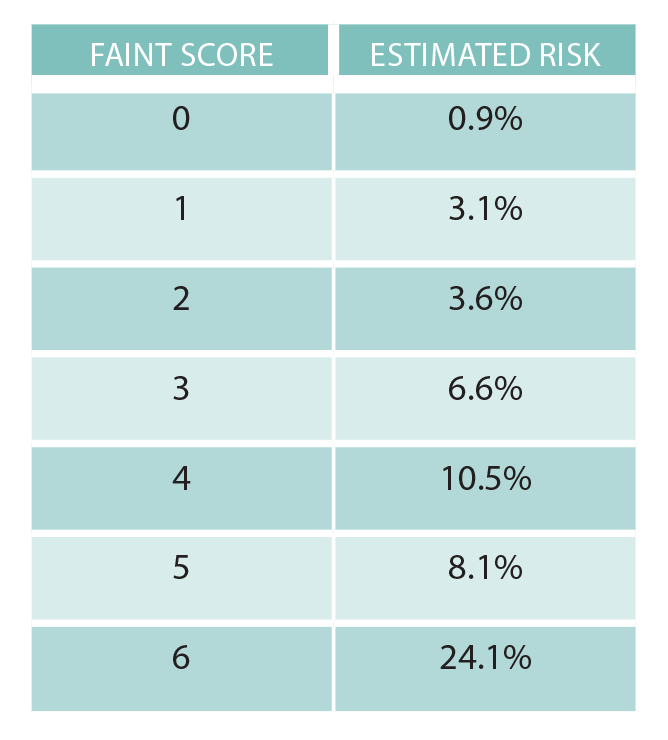
The FAINT Score consists of five variables (see Table 1). A FAINT Score of zero had a sensitivity of over 96 percent and specificity of 22 percent for predicting death or serious cardiac event at 30 days (see Table 1).
The negative predictive value of a FAINT Score of zero was over 99 percent, a promising finding that should satisfy those clinicians who believe that 1 percent is generally an acceptable miss rate for patients presenting with cardiovascular complaints. However, this risk score has not been externally validated and thus is not ready for clinical use in isolation.
The FAINT Score now joins its Canadian cousin from Ottawa, the Canadian Syncope Risk Score. The latter has a greater number of variables (nine), some of which are subjective (ED diagnosis of cardiac syncope, for example), and is designed for use in patients ages 16 and older. Not surprisingly, both scores use the ECG and troponin as important predictive variables.
What’s next? Both scores are pending external validation to confirm that their test characteristics are, in fact, consistent with those in the initial derivation studies. Meanwhile, the formal external validation of the Canadian score is expected to be published soon.
The validation of the FAINT Score is likely a few years away. Until then, we cannot formally endorse the use of it for widespread implementation. However, these scores are an exciting new development in the field of syncope risk stratification and may offer clinicians a useful tool to help determine which patients can be safely discharged directly from the emergency department. Ultimately, we believe these scores should be used in conjunction with, and not instead of, clinical gestalt, as is true for all clinical decision instruments. Consideration of other factors—such as the social circumstances, patient values, and preferences—is always warranted.
Case Resolution
Since the FAINT Score has not yet been externally validated, you cannot rely solely upon it. But its components may still be useful. You aptly order a high-sensitivity troponin and elevated N-terminal-prohormone BNP (NT-ProBNP), both of which come back normal. Calculating the patient’s FAINT Score to be zero, you believe that her risk of a serious cardiac event within 30 days is likely to be less than 1 percent. You return to the bedside and engage in shared decision-making with the patient. She understands that her risk is probably low but not zero. Although she lives alone, she agrees that discharge home with close outpatient follow-up this week is appropriate. The etiology of the syncope is never determined, but months later she is doing well, safely drinking coffee in her living room.
Dr. Probst is associate professor in the department of emergency medicine at Mount Sinai Hospital and Icahn School of Medicine at Mount Sinai in New York City.
Dr. Sun is Perelman Professor and Chair in the department of emergency medicine at the University of Pennsylvania in Philadelphia.
Reference
- Probst MA, Gibson T, Weiss RE, et al. Risk stratification of older adults who present to the emergency department with syncope: the FAINT score [published online ahead of print Oct. 23, 2019]. Ann Emerg Med.
Pages: 1 2 3 | Multi-Page





One Response to “New “FAINT” Score May Work for Syncope Risk Stratification, but Needs Validation”
December 28, 2019
KazmiExcellent. Thanks. -Needs more to add to,it. D/D seizure. Then this. Check orthostatic BP. The best thing is that all ER personnel should start using this and keep on adding things which are necessary to improve this. I am going to start using this and try to improve and add my own pointers.