
A gravid woman presents to your emergency department (ED). Before you can obtain any history, she gives birth in your waiting room. The neonate is apneic and has a heart rate of 48. How do you stabilize this patient?
Explore This Issue
ACEP Now: Vol 43 – No 11 – November 2024Neonatal resuscitation is common; 10 percent of the four million newborns in the U.S. each year will require at least some intervention.1 However, one percent of births will require advanced interventions, including chest compressions, intubation, and medications.2 These rare scenarios are difficult to prepare for; resuscitation guidelines are not strictly followed in more than 90 percent of cases.2 Physicians may experience skill atrophy in these scenarios within two months, underscoring the need for regular review of current guidelines.2
Initial Resuscitation
All necessary personnel and equipment needed for advanced pediatric resuscitation should be present before delivery.4 Immediately after birth, the neonate should be assessed for appearance, pulse, grimace, activity, and respiration (APGAR).5 Cord clamping may be delayed for at least 30 seconds in preterm and term neonates.3 If the neonate is term and has normal tone and breathing and/or crying, they should be placed skin to skin with the mother. Most newborns do not require resuscitative efforts.3
Within 30 seconds, if the newborn has any evidence of apnea, cyanosis, or difficulty breathing, they should be taken to the warmer to maintain a temperature between 36.5–37.5 degrees Celsius and undergo tactile stimulation through drying and rubbing of the back and soles.3,4 Secretions may be cleared and the airway repositioned.3
Advanced Resuscitation
Within 30 seconds of the initial intervention and 60 seconds from birth, the neonate should be reassessed. If the neonate has a heart rate (HR) below 100 or is apneic and gasping, positive pressure ventilation (PPV) should be provided immediately.3 PPV is the most critical step in neonatal resuscitation.2 For every 30 seconds that PPV is delayed, the risk of prolonged admission or death increases by 16 percent.4 A rise in HR is the most important indicator of effective resuscitation. Term infants should initially receive an FiO2 of 0.21 while preterm infants should be started between 0.21 and 0.3, with oxygen titrated based on pulse oximetry. Routine airway suctioning is not recommended. However, if a neonate is delivered through meconium-stained fluid and is showing signs of obstruction during PPV, intubation and tracheal suction can be beneficial.3
PPV is often done incorrectly (Table 1). Two-thirds of cases of continued respiratory depression after resuscitation begins are due to ineffective PPV.2
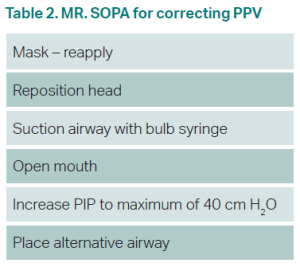
One team member should auscultate HR during the first 15 seconds of PPV. A rising HR is the best indication of effective PPV.3 If there is no increase in HR, PPV may be corrected with the MR. SOPA pneumonic (Table 2).
After 30 seconds of effective PPV, the patient should be reassessed. If HR is 60–99, the MR. SOPA algorithm should be repeated for proper PPV.1 If HR is below 60, chest compressions should be started and an ECG placed.3 The two-hand technique is the most effective. Compressions should be delivered at a ratio of three compressions to one ventilation, for 90 compressions and 30 inflations in one minute.3 Vascular access through an umbilical vein catheter (UVC) should be obtained, although intraosseous (IO) access is acceptable.3
The patient should have an endotracheal (ET) tube placed. ET tube size should be 2.5 mm for neonates under 1,000 grams, 3.0 mm for 1,000–2,000 grams, and 3.5 for neonates over 2,000 grams.1 ET depth is generally “6 + the weight in kilograms,” so a three kg infant would have an ET tube be nine cm at the lip.1 Intubation is difficult; a laryngeal mask airway (LMA) is a useful alternative.2
If the patient is bradycardic after 60 seconds of compressions and ventilations, initiate medications. 0.01–0.03 mg/kg IV epinephrine, or 0.05–0.1 mg/kg through the ET tube, should be given every three to five minutes.3 Volume resuscitation with normal saline or blood may be given at 10 cc/kg over five to 10 minutes in infants with concerns for blood loss.3
In the post-resuscitative state, the patient should be transferred to a higher level of care, where they can be monitored for further complications and undergo therapeutic hypothermia.4 If all steps of resuscitation have been completed and HR remains undetectable 20 minutes after birth, goals of care should be discussed and termination of resuscitation considered.3
 Dr. Turner, originally trained at the Medical University of South Carolina, is an EM intern at Hershey Medical Center in Hershey, Pa.
Dr. Turner, originally trained at the Medical University of South Carolina, is an EM intern at Hershey Medical Center in Hershey, Pa.
 Dr. Sandelich is a pediatric emergency physician at Hershey Medical Center in Hershey, Pa.
Dr. Sandelich is a pediatric emergency physician at Hershey Medical Center in Hershey, Pa.
References
- Sawyer T, Umoren RA, Gray MM. Neonatal resuscitation: advances in training and practice. Adv Med Educ Pract. 2016;8:11-19.
- Garvey AA, Dempsey EM. Simulation in Neonatal Resuscitation. Front Pediatr. 2020;8:59.
- Aziz K, Lee HC, Escobedo MB, et al. Part 5: Neonatal Resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S524-S550.
- Raghuveer TS, Cox AJ. Neonatal resuscitation: an update. Am Fam Physician. 2011;83(8):911-918.
- Finster M, Wood M. The Apgar score has survived the test of time. Anesthesiology. 2005;102(4):855-857.
Pages: 1 2 3 | Multi-Page






No Responses to “Neonatal Resuscitation Tips”