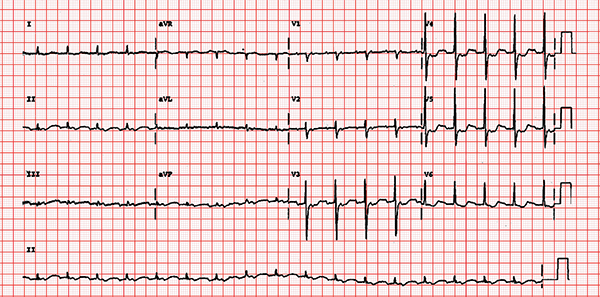
Case: A 19-year-old male arrives at the ED complaining of palpitations. He is known to have supraventricular tachycardia (SVT) and has been in before for the same condition. He is hemodynamically stable, and the electrocardiogram (ECG) shows SVT. Adenosine has worked before, but he asks if there is anything else because it makes him feel awful.
Clinical Question: Is a modified Valsalva maneuver superior to the standard Valsalva maneuver in converting stable patients presenting to the emergency department with SVT to a sinus rhythm?
Background: SVT is a common dysrhythmia seen in patients presenting to the emergency department. There are different ways of restoring patients back to a sinus rhythm (electrical, pharmacologic, and nonpharmacologic). Synchronized cardioversion is usually the treatment of choice in the hemodynamically unstable patient.
A variety of drugs (such as adenosine, calcium channel blockers, and beta blockers) has been used to correct SVT in the hemodynamically stable patient. Adenosine is the drug many people find unpleasant.
The Valsalva maneuver is a noninvasive way to convert patients from SVT to sinus rhythm. It increases the myocardial refractory period by increasing intrathoracic pressure, thus stimulating baroreceptors in the aortic arch and carotid bodies, increasing vagal tone. A systematic review shows this method only works in about one in five patients.1
Relevant Article: Appelboam A, Reuben A, Mann C, et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. Lancet. 2015;386:1747-1753.
- Population: Adult patients presenting to the emergency department with stable SVT (many exclusions were listed in the paper).
- Patients strained for 15 seconds by forced expiration. Immediately after the strain, patients were laid flat, and their legs were elevated by a staff member to 45 degrees for 15 seconds. Patients were then returned to a semi-recumbent position for 45 seconds.
- Comparison: The standard Valsalva maneuver.
- Patients strained for 15 seconds by forced expiration. Patients remained semi-recumbent at 45 degrees.
- Outcome:
- Primary: Return to sinus rhythm at one minute.
- Secondary: Use of adenosine, use of any anti-dysrhythmic, discharge home, length of stay in the ED, and adverse events.
Authors’ Conclusions: “In patients with supraventricular tachycardia, a modified Valsalva manoeuvre with leg elevation and supine positioning at the end of the strain should be considered as a routine first treatment, and can be taught to patients.”
Key Results: There were 428 adult patients included in the study. The mean age was in the mid-50s, approximately 60 percent were female, and about half had a history of SVT.
The modified Valsalva maneuver resulted in an increased frequency of conversion out of SVT to sinus rhythm compared to the standard Valsalva maneuver. The adjusted odds ratio = 3.7 (95 percent CI, 3.3–5.8; P<0.0001). Number needed to treat (NNT) = 4 (95 percent CI, 3–7).
Primary Outcome: Return to sinus rhythm at one minute:
Modified 43 percent versus standard 17 percent, NNT = 4
There was less use of adenosine and anti-dysrhythmic drugs. There was no difference in length of stay in the ED, discharge home, or adverse events.
The modified Valsalva maneuver resulted in an increased frequency of conversion out of SVT to sinus rhythm compared to the standard Valsalva maneuver.
EBM Commentary:
- This pragmatic study was very well done and addressed a common condition presenting to the ED. The postural modification of the standard Valsalva maneuver represents an inexpensive, well-tolerated treatment option with a NNT of 4.
- Blinding was a potential limitation in this study. The authors tried hard to minimize this type of bias. It was not possible to blind the providers to the treatment group. However, the patients were not aware of which treatment was the modified technique. The independent cardiologist who retrospectively assessed the ECGs was blinded to group allocation. If there were disagreements about ECG interpretation between the unblinded treating physician and the blinded cardiologist, an independent electrophysiologist, also blinded, arbitrated.
Bottom Line: To REVERT your next stable patient with SVT to a sinus rhythm, consider a postural modification of the standard Valsalva maneuver.
Case Resolution: You use the modified Valsalva maneuver and successfully convert him to a sinus rhythm.
Thank you to Dr. Robert Edmonds, a third-year emergency medicine resident at the University of Missouri at Kansas City, for his help on this review.
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.
References
- Smith GD, Dyson K, Taylor D, et al. Effectiveness of the Valsalva manoeuvre for reversion of supraventricular tachycardia. Cochrane Database Syst Rev. 2013 Mar 28;3:CD009502.
Pages: 1 2 3 | Multi-Page






2 Responses to “Modified Valsalva Maneuver Better Way to Manage Supraventricular Tachycardia”
June 19, 2016
Chuck PilcherI’ve found occasional success with an even more aggressive “modification” of the Valsalva maneuver.
The goal of the maneuver is to raise pressure on the carotid baroreceptors, right? So if the “regular” Valsalva maneuver hasn’t worked, I’ve had (usually young, athletic) patients) lie prone on the gurney, hang their head over the end of that gurney so they are at a 90 degree angle head-down, take a deep breath and hold it for 15 seconds or so. It seems to work better.
May 30, 2019
joeNice article. I want to add more.
I believe A normal heart beats 60 to 100 beats per minute (bpm) but when you have SVT, your heart rate may be sustained way above 100 bpm, sometimes up to 180 or 200bpm, for several minutes or hours. You may feel that you have a racing heartbeat, which can be described as palpitations.