The Case

Explore This Issue
ACEP Now: Vol 36 – No 12 – December 2017French surgeon Jacques Lisfranc de St. Martin, for whom the Lisfranc joint and Lisfranc fracture are named.
Painting by an unspecified artist; photo by Pierre Petit, Public Domain
A 24-year-old male presents to the emergency department after sustaining an injury to his right foot during football practice the previous day. He states he was viciously tackled while sprinting across the field. After falling on a plantar-flexed, fixed foot, he felt a snap in the center of his foot and developed immediate pain and swelling over the dorsum of his foot. On physical exam, there is maximal swelling over the first and second tarsometatarsal joints, and he is unable to bear weight.

Introduction
The midfoot is composed of the cuboid, navicular, and three cuneiform bones, which form the arch of the foot. The Lisfranc joint complex is composed of the bones and ligaments that connect the midfoot to the five metatarsals of the forefoot.1 The Lisfranc ligament connects the base of the second metatarsal to the lateral aspect of the medial cuneiform (see Figures 1 and 2).1,2 This oblique ligament is what provides stability to the joint, despite the absence of a ligamentous connection between the first and second metatarsal.
The annual incidence of Lisfranc injuries is 1 in 55,000 persons per year.3 These injuries can be difficult to recognize and are most commonly misdiagnosed as an ankle sprain on initial visit to the emergency department. Undiagnosed cases can result in long-term misalignment and functional weight-bearing difficulties. Therefore, it is important to keep a high index of suspicion and perform a detailed physical exam. Also, keep in mind that 20 percent of Lisfranc joint injuries are missed on initial radiograph.3
What Is the Mechanism of Injury?
These injuries can result from a direct crush mechanism or high-velocity blunt trauma, such as from a motor vehicle accident. However, the injury most commonly occurs indirectly from extreme plantar flexion with rotation of the ankle, during which the second metatarsal is prone to dislocate dorsally if an axial load is applied at the same time.3 Examples include falling from a horse with the foot caught in the stirrup, stepping off a curb, or planting your foot in a hole.
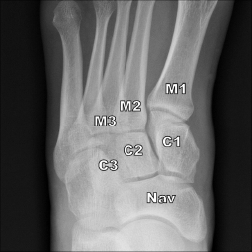
Figure 1: Normal AP weight-bearing radiograph of the left midfoot showing first metatarsal base (M1), second metatarsal (M2), third metatarsal (M3), medial cuneiform (C1), middle cuneiform (C2), lateral cuneiform (C3), and navicular bone (Nav). Note that there is less than 2 mm between C1 and M2 and between M1 and M2.
Credit: Siddiqui N A, Galizia M S, Almusa E, et al. RadioGraphics. 2014;34(2):514-531.
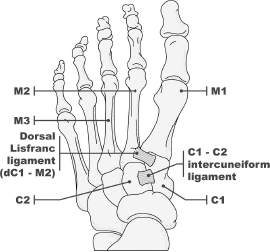
Figure 2: The Lisfranc ligament connects the base of the second metatarsal to the lateral aspect of the medial cuneiform.
Credit: Siddiqui N A, Galizia M S, Almusa E, et al. RadioGraphics. 2014;34(2):514-531.
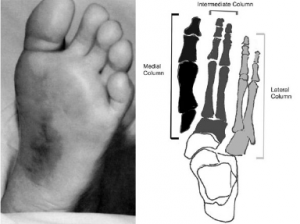
Figure 3: Left: Plantar ecchymosis. Right: Medial, intermediate and lateral column associated with midfoot biomechanics.
Emerg Med J. 2017;34:52-56.
Physical Exam Suggestive of Lisfranc Fracture
- Inability to bear weight or stand on tiptoes.2
- Ecchymosis on medial plantar aspect of foot is pathognomonic but may be absent in minor fractures (see Figure 3).2
- Dorsal midfoot pain and swelling.
- Pain elicited with passive supination and pronation of the forefoot with the hindfoot held fixed.4

Figure 4A: Initial AP non-weight-bearing radiograph shows normal alignment of the medial and middle columns of an 11-year-old boy after a fall.
Credit: Siddiqui N A, Galizia M S, Almusa E, et al. RadioGraphics. 2014;34(2):514-531.

Figure 4b: AP weight-bearing radiograph shows widening of the joint seen as a gap of more than 2 mm between C1 and M2 and between M1 and M2 (arrow).
Credit: Siddiqui N A, Galizia M S, Almusa E, et al. RadioGraphics. 2014;34(2):514-531.

Figure 6: AP weight-bearing radiograph showing a small chip fracture from medial margin of base of M2, known as the “fleck sign.”
Credit: Siddiqui N A, Galizia M S, Almusa E, et al. RadioGraphics. 2014;34(2):514-531.
Diagnosis
Obtain three view radiographs of the foot (anteroposterior [AP], lateral, and standard 45-degree oblique views). Ideally, weight-bearing stress views should be obtained since initial plain X-rays may fail to show subtle widening of the articulation spaces (See Figure 4).1 Consider a CT scan of the foot if X-rays do not show an injury but you remain highly suspicious.
Normal Three-Column Anatomy of Lisfranc Complex on X-Ray (see Figures 1 and 5)
- On the AP view, the medial edge of the base of the second metatarsal (M2) should line up with the medial edge of the middle cuneiform (C2).1
- The gap between the second metatarsal and medial cuneiform is <2 mm.
- On the oblique view, the medial edge of the third and fourth metatarsal should line up with the medial edges of the middle cuneiform and cuboid, respectively.1
- On the lateral view, the superior border of the first metatarsal (M1) should align with the superior border of the medial cuneiform (C1).

Figure 5: Normal three-column anatomy of Lisfranc complex. A shows the AP view.
Dr. Anton Helman/Emergency Medicine Cases

B shows the oblique view.

C shows the lateral view.
Diagnostic Imaging for the Emergency Physician. Elsevier 2011
X-Ray Findings Suspicious for Lisfranc Injuries
- On the AP view, widening of >2 mm between the base of the first and second metatarsal indicates instability (See Figure 4).1
- “Fleck sign” is pathognomonic for a Lisfranc injury. This is a small bony fragment avulsed from the second metatarsal base or medial cuneiform (see Figure 6).1
Management
Stable dislocation/fracture injuries are defined as having less than 2 mm of displacement between the first metatarsal and medial cuneiform. These can be managed non-operatively with reduction and casting.5 The patient should be placed in a non-weight-bearing below-the-knee cast for six weeks and have outpatient orthopedic follow-up in two weeks.6
For unstable fractures and dislocations, immediate orthopedic consultation is needed for surgical intervention with internal fixation.5 After surgery, immobilization and non-weight-bearing status is recommend for eight to 12 weeks.7 The screws may then be removed at 12 weeks.7 Full weight-bearing is typically not permitted until all hardware is removed.
 Dr. Paez Perez is an emergency medicine resident at St. Joseph’s Regional Medical Center in Paterson, New Jersey.
Dr. Paez Perez is an emergency medicine resident at St. Joseph’s Regional Medical Center in Paterson, New Jersey.
References
- Siddiqui NA, Galizia MS, Almusa E, et al. Evaluation of the tarsometatarsal joint using conventional radiography, CT, and MR imaging. Radiographics. 2014;34(2):514-531.
- Lau S, Bozin M, Thillainadesan T. Lisfranc fracture dislocation: a review of a commonly missed injury of the midfoot. Emerg Med J. 2017;34(1):52-56.
- Caswell F, Brown C. Identifying foot fractures and dislocations. Emerg Nurse. 2014;22(6):30-34.
- Englanoff G, Anglin D, Hutson HR. Lisfranc fracture-dislocation: a frequently missed diagnosis in the emergency department. Ann Emerg Med. 1995;26(2):229-233.
- Anderson RB, Hunt KJ, McCormick JJ. Management of common sports-related injuries about the foot and ankle. J Am Acad Orthop Surg. 2010;18(9):546-556.
- Buzzard BM, Briggs PJ. Surgical management of acute tarsometatarsal fracture dislocation in the adult. Clin Orthop Relat Res. 1998;(353):125-133.
- Harwood MI, Raikin SM. A Lisfranc fracture-dislocation in a football player. J Am Board Fam Pract. 2003;16(1):69-72.
Pages: 1 2 3 | Multi-Page





No Responses to “Identify and Treat Lisfranc Injuries”