Explore This Issue
ACEP Now: Vol 40 – No 03 – March 2021The Case
A 15-year-old boy presents to the emergency department with acute left knee pain. While playing football, he was tackled with his left knee planted and experienced a sudden pain. He was unable to ambulate after the injury. On exam, he is in severe discomfort and tachycardic and has an obvious deformity of his left knee.
Discussion
Patellar dislocations and knee dislocations, though often mistakenly used interchangeably, are different clinical entities with distinct mechanisms and presentations.
Patellar dislocation occurs when there is disarticulation of the patella bone from the patellofemoral joint. It usually occurs from low-to-moderate trauma sustained during sports or other physical activity. Risk factors for patellar dislocation include structural variants of the patella or femoral trochlea, ligamentous laxity, trauma, and connective tissue disorders. Patellar dislocations represent 3 percent of knee injuries, with a high recurrence rate ranging from 15 to 44 percent for first-time dislocations and 50 percent with a previous history of two or more dislocations.1,2 The risk of patellar dislocation injury is highest in females ages 10 to 17 years old, with an incidence of 29 per 100,000.2 The mechanism in the vast majority of patellar dislocations is noncontact involving knee flexion, a valgus force with external rotation. Patients with patellar instability can struggle to return to sports and develop functional limitations, arthritis, and chronic pain.1,2
Knee dislocation is a dislocation of the tibia with respect to the femur and is seen in high-energy traumas including motor vehicle accidents, falls from heights, industrial injuries, and sports injuries, as well as spontaneously in the morbidly obese during ambulation.3 Knee dislocations involve disruption of major knee-stabilizing ligaments (medial collateral ligament, posterior cruciate ligament, anterior cruciate ligament, lateral collateral ligament, and posterolateral corner). Meniscal tears are seen in about 50 percent of cases, and fractures are seen in about one-third of cases.4,5 Knee dislocations are substantially less common than patellar dislocations, with slightly higher incidence in males and a mean patient age of 35.6 Anterior knee dislocations are more common and account for 40 percent of all knee dislocations.7 We will discuss key differences between these injuries, their complications, and respective ED management.
Anatomy and Biomechanics

Figure 3: Visible lateral deviation of the patella. Credit: Radiographics. 2010;30(4):961-981.
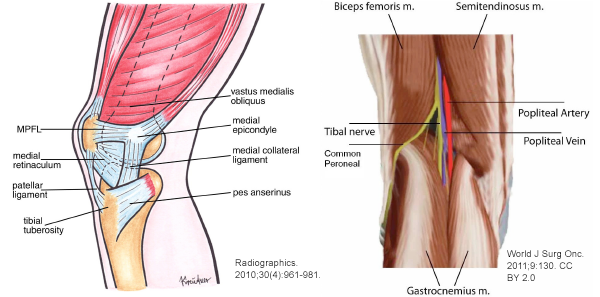
The patella acts as a lever arm connecting the quadriceps muscles via the quadriceps tendon to the tibia via the patellar tendon. Collectively, this unit is responsible for knee extension and is often referred to as the “extensor mechanism.” The patellofemoral joint refers to the articulation of the patella within the trochlear groove of the femur. Patellar instability can be derived from any anatomical change in the patellofemoral joint. The vastus medialis obliquus muscle and medial patellofemoral ligament (MPFL) are responsible for much of the medial stability of the patellofemoral joint by counteracting the natural lateral glide of the patella (see Figure 1).8
Knee dislocations are associated with more dangerous complications because injuries involving this structural complex can be associated with vascular and/or nerve injury. The primary stabilizer ligaments of the posterolateral corner are the popliteus tendon, fibular collateral ligament, and popliteofibular ligament. Both the long and short head of the biceps femoris muscle act as secondary stabilizers here.9 Running through the popliteal fossa at the level of the tibiofemoral junction are the popliteal artery and vein, tibial nerve, and common fibular (peroneal) nerve (see Figure 2).
Pathophysiology
In 93 percent of patellar dislocations, the mechanism involved is a flexion and valgus movement of the knee without direct contact. Noncontact mechanisms often involve a twisting injury with the foot externally rotated and the knee extended, while traumatic causes typically involve a direct blow to the knee. There are also a number of predisposing factors that increase risk of patella dislocation in individuals. One such risk factor is trochlear dysplasia, where the trochlear groove is flat or convex as a result of gradual filling of the trochlear floor.10 Another predisposing factor to patellar dislocation is a high-riding patella (patella alta). When the patellar tendon is too long, the patella bone sits superior to the trochlear fossa.11
Knee dislocation usually requires higher-energy mechanisms. However, a low-energy dislocation mechanism has been documented in patients with morbid obesity. Popliteal artery injury is reported in 18 to 64 percent of knee dislocations, with 12 percent of these cases requiring amputation. The amputation rate in patients with popliteal ischemia for greater than eight hours is 86 percent, thus early intervention is crucial if this diagnosis is suspected.12,13 Peroneal nerve injury is another potential complication. Nerve injury is seen in 25 to 33 percent of knee dislocations and is more commonly seen in sports-related injuries.14 It is worth noting that knee dislocations, with or without spontaneous reduction, may present with other significant traumatic and life-threatening pathology.
Clinical Features and Physical Exam
In the majority of patellar dislocation cases, the patient will have subluxed or dislocated with spontaneous reduction prior to arrival to the emergency department. Thus, it is critical to clarify the mechanism of injury and symptoms prior to arrival. Only 20 percent of patellar dislocations require reduction in the emergency department.10 In patients whose dislocations do not resolve spontaneously, most will be evident with visible lateral deviation of the patella (see Figure 3).
Most patients present in obvious discomfort, often with the knee held in slight flexion. A joint effusion may be present. Distally, the patient should be neurovascularly intact as the popliteal bundle is posterior to the femorotibial joint and unaffected by this injury. It is important to confirm the quadriceps and patellar tendons are intact by assessing active and passive leg raise against gravity and/or with point-of-care ultrasound. Clinical exam findings that suggest a subluxation or spontaneous dislocation reduction prior to arrival include tenderness of the medial femoral condyle (attachment site of the MPFL) or lateral femoral condyle (where the patella likely collided with the lateral femur during the event).
Knee dislocations can be clinically obvious with a significant mechanism and gross deformity. However, many knee dislocations spontaneously reduce, and about 50 percent appear normal with no obvious deformity on initial presentation.15 Given that this injury often involves high-energy mechanisms, it is important to evaluate for other injuries. If a patient presents with acute trauma to the knee, it is important to evaluate for more subtle signs such as joint effusion, swelling, and ecchymosis. In an acute knee dislocation, there may be a dimple sign or buttonholing of the medial femoral condyle through the capsule. Structural examination of the major knee ligaments should be performed, including anterior and posterior drawer test and varus and valgus stress test, at minimum. All lower-extremity pulses should be assessed and documented when there is concern for knee dislocation due to possible injury to the popliteal artery, which is the most feared complication. Early recognition and intervention for this vascular injury is associated with decreased likelihood of complications. Vascular injury resulting from knee dislocation can present as a pulseless lower extremity. Conversely, the presence of peripheral pulses in the lower extremity alone does not exclude a vascular injury, so serial vascular exams must be performed.15 Other signs of vascular injury can include pallor, cold limb, ecchymosis, and paresthesia. If vascular injury is suspected or confirmed, vascular surgery should be consulted immediately. Even if this injury spontaneously reduces before presentation to the emergency department, the risk of vascular injury remains. To assess for nerve injury, a motor and sensory exam should be performed and documented. With peroneal nerve injury, weakness of ankle dorsiflexion, or “foot drop,” is most common. There may also be numbness or paresthesia along the lateral leg and dorsum of the foot.16
Imaging
Standard radiographs are indicated for both patellar and knee dislocations. In the case of patellar dislocation, pre-reduction radiographs may not be required at the discretion of the physician and based on confidence in diagnosis. Standard post-reduction radiographs of the knee should be obtained for both entities. For patellar dislocation, imaging is typically normal but may demonstrate avulsion fractures or loose bodies (see Figure 4).

Figure 4: X-ray of avulsion fractures/loose
bodies in patellar dislocation. Credit: John Kiel

Figure 5: X-ray of dislocated femorotibial
joint in a knee dislocation. Credit: John Kiel

Figure 6: X-ray showing
widened joint space. Credit: John Kiel
Point-of-care ultrasound can also rapidly evaluate the patellofemoral joint and extensor mechanism. Radiographs of a knee dislocation may show a clearly dislocated femorotibial joint (see Figure 5), which correlates to the physical exam.
In cases where spontaneous reduction occurred prior to arrival, radiographs can be normal. Other findings may show widened joint space (see Figure 6), fracture, or hemarthrosis.
Consideration of vascular imaging is critical for all known or suspected knee dislocations. If there is evidence of an ischemic limb post-reduction, vascular surgery should be consulted for immediate transfer to the operating room. If the limb is well perfused but with an absent or asymmetrical pulse, CT angiography to assess for vascular injury is indicated. If the limb is well perfused and pulse is present, an Ankle Brachial Index (ABI) should be assessed. If the ABI is <0.9, CT angiography is indicated. If the ABI is ≥0.9, the patient should be admitted for 24-hour observation with serial vascular exams.17
Pre-reduction imaging of a knee dislocation is indicated in patients with good bilateral pulses to assess for concomitant fracture. If there is evidence of fracture, CT is recommended to further evaluate for preoperative planning.18
Rarely, this injury can occur in a patient following a total knee arthroplasty (TKA) (see Figure 7). This is most commonly seen in TKAs that retain the posterior cruciate ligament. Prevalence of this complication is low, at 0.15 to 0.5 percent.19 Reduction should occur in the operating room under general anesthesia, and in most cases, a complete surgical revision or an intercondylar constrained design is indicated.
Reduction and Disposition
In patients with patellar dislocation where spontaneous reduction has not occurred, the patella should be manually reduced. The analgesic approach is at the discretion of the physician; however, the reduction is often quick and easy to perform if the patient is willing, not requiring significant analgesia or procedural sedation. However, if it is anticipated that the patient’s level of pain or anxiety will make the reduction more difficult, a small amount of analgesia may be used.20 Simple reassurance, calming of the patient, and education on the reduction process are important. Here’s how to reduce a lateral patellar dislocation:20
- Position the patient supine, in the seated position with hips in slight flexion (to prevent patellar tendon contraction).
- Use one hand to maintain support near the ankle.
- While applying medial pressure to the lateral patella, passively extend the knee slowly.
- The physician should note a click as the patella slides back into the femoral groove.
- Confirm with post-reduction anteroposterior and lateral radiographic views.
Post-reduction, the patient should be placed in a knee immobilizer to take away the flexion and extension mechanism of the knee. They should be non-weight-bearing (using crutches). All physical activity and sporting events are prohibited until cleared by orthopedics at follow-up. Most uncomplicated first-time dislocations can be managed nonoperatively with physical therapy and a slow return to play. Recurrent or complicated dislocations involving osteochondral injuries or instability can require elective surgical intervention.
Reduction of a knee dislocation should be attempted with procedural sedation in consultation with orthopedic surgery if possible. The first attempt should involve simple longitudinal traction. If this is unsuccessful, the next step is to attempt to reverse the direction of the deforming force:18
- In an anterior knee dislocation, push the tibia posterior while simultaneously lifting the distal femur.
- In a posterior knee dislocation, lift the tibia anteriorly while simultaneously placing pressure over the femur.
- If these reduction techniques are unsuccessful, operative management under anesthesia is indicated.
Post-reduction, radiographs should be obtained immediately to confirm a successful reduction, and the patient should be placed in a splint at 20 degrees of flexion. The splint should be constructed such that posterior subluxation of the tibia is prevented while also minimizing vascular traction. The splint should be windowed to allow for repeat vascular exams of the foot.18
Summary

Figure 7: X-ray showing knee dislocation in a patient with a total knee arthroplasty. Credit: John Kiel
Understanding the differences between patellar and knee dislocations is imperative for recognizing and preventing potentially catastrophic complications (see Table 1). Patellar dislocation is an injury that occurs most commonly in young and active individuals. The majority of patellar dislocations will reduce spontaneously prior to ED arrival. Knee dislocation is an injury that can present similarly and should be in the considered differential diagnosis based on mechanism, examination, and clinical gestalt. This injury usually involves high-energy mechanisms. About 50 percent of cases will reduce spontaneously prior to ED arrival, thus a thorough knee examination is critical; careful neurovascular evaluation of the lower-extremity status must be performed. If there is evidence of vascular injury, the patient requires emergent revascularization with vascular surgery, as ischemia time is correlated with risk of amputation.
In the emergency department, reduction of patellar dislocations is generally straightforward. Post-reduction radiographs should be obtained and the patient placed in a knee immobilizer. This injury does not require orthopedic consultation in the emergency department; however, patients should follow up with orthopedic surgery as an outpatient within one to two weeks. Return to play should be individualized toward the athlete and the activity, but main treatment goals prior to return to play are lower-limb stabilization, strengthening of the quadriceps and gluteus medius muscles, and avoidance of specific high-risk movements. Knee dislocation reduction in the emergency department typically requires simple longitudinal traction with pre- and post-reduction radiographs and neurovascular exam. Post-reduction testing typically involves an ABI and often a CT angiogram. All patients with knee dislocations require orthopedic consultation in the emergency department and often vascular/trauma services as well. The affected extremity should be splinted at 20 degrees, and the patient should be admitted for 24-hour observation with serial vascular exams. In follow-up, the patient may require staged reconstruction or repair of the injured ligaments and other soft tissue structures.
Table 1: Comparison of Patellar Dislocation and Knee Dislocation
| Patellar Dislocation | Knee Dislocation | |
|---|---|---|
| Mechanism | Noncontact twisting injury (flexion with external rotation) or direct blow (often sports-related) Anatomical risk factors |
High-energy mechanisms (eg, trauma, motor vehicle accidents, sports) Morbid obesity |
| Physical Exam | Majority spontaneously reduce Painful laterally displaced patella Neurovascularly intact |
50% spontaneously reduce Painful anterior, posterior, or lateral disarticulation of femur and tibia Structural examination of knee Assess neurovascular status |
| Complications | Recurrent dislocations Patellofemoral pain or arthritis Osteochondral defect |
Arthrofibrosis (most common) Popliteal artery injury Amputation Peroneal nerve injury Chronic pain or persistent knee instability |
| Imaging | Pre-reduction radiographs: if fracture suspected Post-reduction radiographs: always |
Pre-reduction radiographs to assess for concomitant fracture Post-reduction radiographs Well perfused with absent/asymmetric pulse: CT angiography Well perfused with normal pulse: Ankle Brachial Index (ABI) |
| Reduction | Pre-reduction analgesia or sedation not typically required Apply medial pressure to the lateral patella, passively extend the knee slowly |
Requires procedural sedation Attempt simple longitudinal traction first If fails, reverse direction of the dislocation If both fail, move to operating room for reduction under anesthesia Post-reduction neurovascular assessment |
| Management | If subluxated, reduce and obtain post-reduction radiograph If reduced prior to emergency department, confirm extensor mechanism intact (have patient extend leg or evaluate via ultrasound) Place in knee immobilizer |
Reduce under procedural sedation Post-reduction ABI or CT angiography based on pulse status If evidence of vascular injury or hard signs of ischemia, move to operating room and obtain vascular surgery consult immediately (do not delay for imaging) If no emergent vascular injury, place in splint at 20 degrees flexion, admit for 24-hour observation with serial exams |
| Consultation | Does not require orthopedic consultation in the emergency department | Requires orthopedic consult and often vascular/trauma services |
| Disposition | Discharge home and counsel on complications, return-to-play goals Outpatient orthopedic follow-up in 1–2 weeks |
Admit for serial examinations based on consult discretion |
Case Resolution
The patient’s deformity was consistent with a laterally dislocated patella. The limb was well perfused, with no neurovascular insult. The injury was successfully reduced in the emergency department after administration of IV fentanyl. A knee immobilizer and crutches were provided. Outpatient follow-up with orthopedic surgery and physical therapy was arranged.
Christian Casteel is EMRA Medical Student Council southcentral representative and a medical student at Kansas City University of Medicine and Biosciences.
Dr. Kiel is assistant professor of emergency medicine and sports medicine at University of Florida College of Medicine–Jacksonville.
References
- Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114-1121.
- Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations. The natural history. Am J Sports Med. 1986;14(2):117-120.
- Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59(2):236-239.
- Marin EL, Bifluco SS, Fast A. Obesity. A risk factor for knee dislocation. Am J Phys Med Rehabil. 1990;69(3):132-134.
- Yu JS, Goodwin D, Salonen D, et al. Complete dislocation of the knee: spectrum of associated soft-tissue injuries depicted by MR imaging. AJR Am J Roentgenol. 1995;164(1):135-139.
- Ménétrey J, Putman S, Gard S. Return to sport after patellar dislocation or following surgery for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2320-2326.
- Arom GA, Yeranosian MG, Petrigliano FA, et al. The changing demographics of knee dislocation: a retrospective database review. Clin Orthop Relat Res. 2014;472(9):2609-2614.
- Smirk C, Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10(3):221-227.
- Richter M, Bosch U, Wippermann B, et al. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocation. Am J Sports Med. 2002;30(5):718-727.
- Duthon VB. Acute traumatic patellar dislocation. Orthop Traumatol Surg Res. 2015;101(1 Suppl):S59-67.
- Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics. 2010;30(4):961-981.
- LaPrade RF, Ly TV, Wentorf FA, et al. The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med. 2003;31(6):854-860.
- Medina O, Arom GA, Yeranosian MG, et al. Vascular and nerve injury after knee dislocation: a systematic review. Clin Orthop Relat Res. 2014;472(9):2621-2629.
- Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59(2):236-239.
- Meyers MH, Harvey Jr JP. Traumatic dislocation of the knee joint. A study of eighteen cases. J Bone Joint Surg Am. 1971;53(1):16-29.
- Ng JWG, Myint Y, Ali FM. Management of multiligament knee injuries. EFORT Open Rev. 2020;5(3):145-155.
- Kiel J. Knee dislocation. WikiSM website. Accessed Feb. 26, 2021.
- Lezak B, Massel D. Peroneal nerve injury. StatPearls website. Accessed Feb. 26, 2021.
- Boyce RH, Singh K, Obremskey WT. Acute management of traumatic knee dislocations for the generalist. J Am Acad Orthop Surg. 2015;23(12):761-768.
- Wolfe S, Varacallo M, Thomas J, et al. Patellar instability. StatPearls website. Accessed Feb. 26, 2021.





No Responses to “How To Identify and Treat Patellar Dislocation Versus Knee Dislocation”