
Explore This Issue
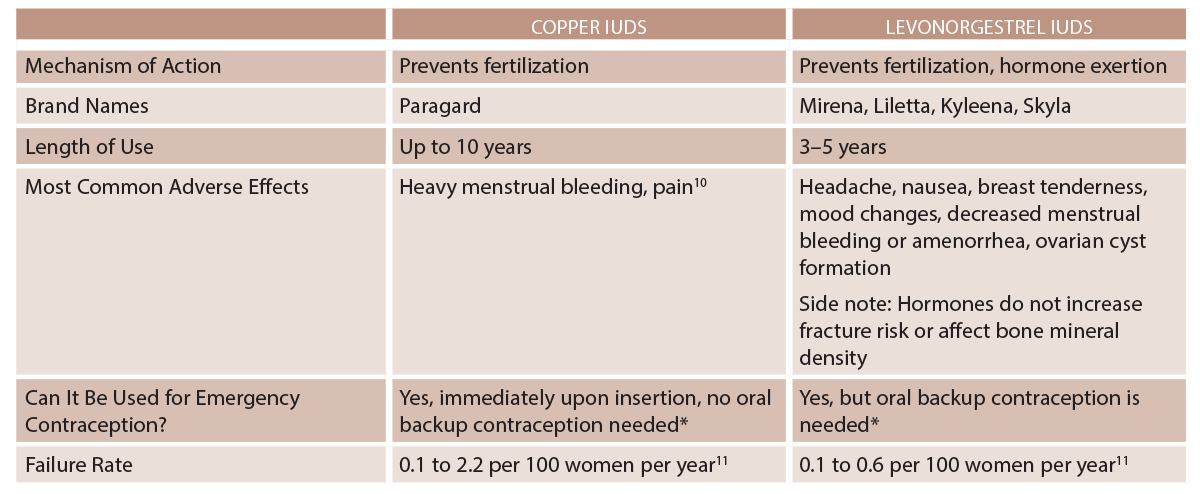
ACEP Now: Vol 38 – No 09 – September 2019(click for larger image) Table 1: IUD Types
* Immediately after an abortion, childbirth, or transitioning contraceptive methods.1
Pelvic Inflammatory Disease
Risk of pelvic inflammatory disease (PID) is elevated in the first three weeks following IUD insertion, before returning to baseline rates.4,8 IUD insertion is contraindicated in women with current purulent cervicitis or known chlamydial/gonorrheal infection until treatment is complete and symptoms have resolved.1,8 If PID is diagnosed in an individual with an IUD in place, Centers for Disease Control and Prevention (CDC) guidelines recommend leaving the IUD in place (outcomes are similar whether the IUD is removed or left in place).4 PID should be treated the same as in patients without IUDs in place and requires follow-up within 48 to 72 hours to assess for clinical improvement. If clinical improvement fails to occur, IUD removal should then be considered.5 There are currently no CDC recommendations on management of tubo-ovarian abscess in a woman with an IUD. Current protocols call for inpatient treatment with IV antibiotics, with consideration of IUD removal if clinical improvement is not observed.5
Expulsion
If expulsion is suspected, pelvic exam should be performed to assess for the IUD strings or a partially expelled IUD protruding out of the cervical os.5 If the IUD and strings are not present, imaging such as an ultrasound, abdominal radiograph, or CT should be obtained for IUD localization and potential perforation. If the IUD cannot be located, it may have been fully expelled. See Table 2 for information on expulsion risk.
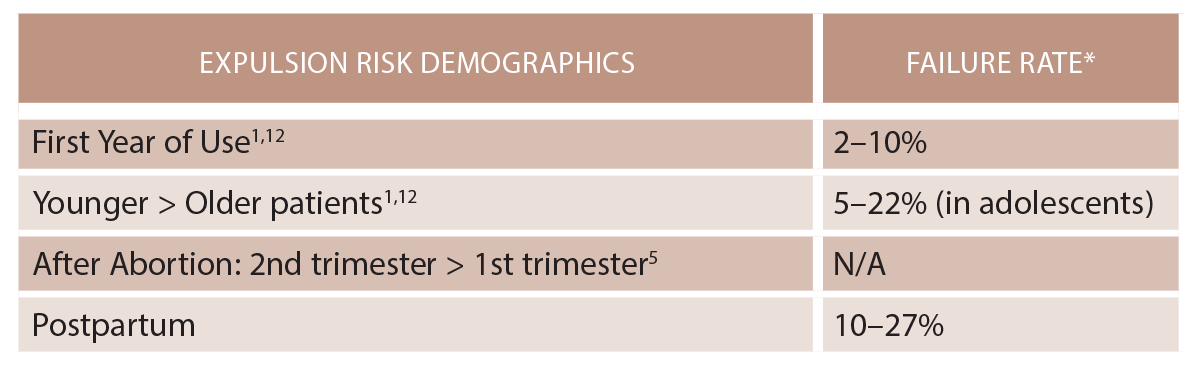
(click for larger image) Table 2: IUD Expulsion
* Failure rate range is 0.1 to 2.2 per 100 women years.11
Perforation
Uterine perforation is a potentially serious complication of IUD use and can lead to invasion and migration to abdominal and pelvic organs. The IUD may be embedded in the myometrium or translocate through the uterus to the abdominal cavity. Migration to adjacent organs can lead to bowel obstruction, peritonitis, fistula formation, obstructive uropathy, and intraperitoneal adhesions.3
Primary perforation occurs during insertion and is typically associated with severe abdominal pain.3 Secondary perforation is a delayed event and can present as chronic abdominal pain, vaginal bleeding, missing strings, or even asymptomatically.3 The incidence of uterine perforation is estimated at between 0.2 and 3.6 per 1,000 insertions.2
Imaging for IUD localization should be performed with ultrasound, abdominal X-ray, and/or CT scan. Eighty percent of IUDs are found in the peritoneal cavity after perforation.3 There is no substantial difference in prevalence of perforation between levonorgestrel and copper IUDs; adhesions are more highly associated with copper IUDs.2,9 Risk factors for uterine perforation include breastfeeding, postpartum state, lack of experience by the health care provider performing insertion, extreme anteflexion or retroflexion of the uterus or uterine abnormalities, multiparity, nulliparity, history of cesarean delivery, and myomectomy.9 Patients may require hysteroscopy, cystoscopy, colonoscopy, laparoscopy, or exploratory laparotomy depending on IUD location.
Pages: 1 2 3 4 | Single Page




No Responses to “How to Approach Patients Who Have an Intrauterine Device”