
Explore This Issue
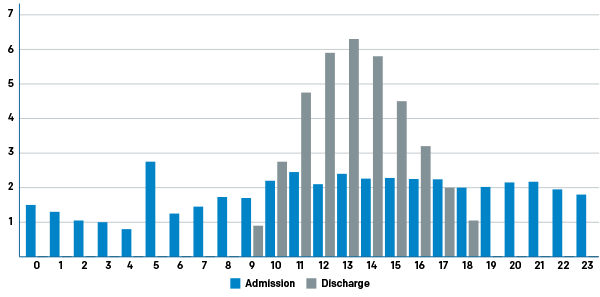
ACEP Now: Vol 40 – No 07 – July 2021Figure 1: Typical Hospital Disequilibrium by Hour of the Day
Shifting the discharge curve to the left has a number of positive effects. It creates capacity earlier in the day and smooths the workflow of the team.
Every inpatient bed falls prey to inefficiency due to suboptimally designed operations and processes. Patients no longer needing medical beds continue to occupy them due to process and system failures. Some of the contributors to this squandered capacity are:11–13
- Waiting for transportation
- Waiting for durable medical equipment
- Waiting for medications
- Waiting for a physician’s order to be written
- Waiting for the nurse to provide education
- Waiting for a skilled nursing facility (SNF) or rehabilitation facility bed placement
Hospitalists have become the busiest admitting service in most hospitals across the country, and beds for hospitalist service patients are often the tightest. Facilities that adhere to strict hospital geography by service often find themselves with even more difficulty placing admitted patients because an available bed may not belong to the service or the team to whom the patient has been admitted, creating yet another fixable barrier contributing to boarding.
Improving Discharge Rates
Though many hospitals have employed early discharge orders (eg, by 10 a.m.) as a performance metric for inpatient clinicians (particularly hospitalists), this typically does not translate into an empty clean bed for several hours. Many institutions are tracking true empty beds using a discharge by noon (DBN) metric, which better reflects efficient operations and processes around discharge. Inpatient care is a team sport, and a patient discharge requires a cast of characters touching the patient, including bedside nurses, physical therapists, pharmacists, and case managers. Achieving great DBN numbers requires strong teamwork.
Early discharges don’t happen without a concerted effort. To avoid readmission, patients need education, medication, durable medical equipment, follow-up appointments, and safe transportation home. Often a physical therapy evaluation is necessary to identify whether the patient is a fall risk at home.
All this planning requires coordination. Care coordination (also called case management) is a newer discipline, and care coordinators or case managers have become indispensable members of inpatient health care teams. These team members can be nurses or social workers. More mature departments have separated utilization review from case management and have identified more experienced workers to manage patients with complicated dispositions. Typically, it is harder to get patients going to SNFs or rehabilitation centers discharged early, though it varies by institution. Though it is not the whole story, many hospitals are focusing on the patients being discharged to home for the best results in DBN. That’s because the flow of these patients is the least dependent on factors that are out of the inpatient team’s control.
An evolving body of research describes strategies that can help increase DBN by addressing the barriers listed above. Strategies to increase early discharges include:
Pages: 1 2 3 4 5 | Single Page






No Responses to “Hospital-Wide Strategies for Reducing Inpatient Discharge Delays and Boarding”