[/fullbar]
Explore This Issue
ACEP Now: Vol 38 – No 03 – March 2019Common Emergency Department Application
Structure: Retina
Evaluate for: Retinal Detachment
The retina is a crucial structure to evaluate for patients with visual complaints. In a normal eye, the retina cannot be distinguished from the other posterior layers, appearing as one homogenous structure.2 The retina is anchored at the ora serrata laterally and the optic nerve posteriorly. This will be important later on when distinguishing retinal versus vitreous detachments.
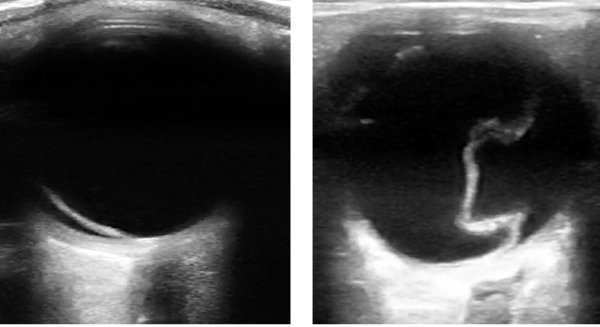
Figure 6 (LEFT): In retinal detachment, the retinal membrane will be lifted off of the posterior or lateral globe and appear as a hyperechoic (bright white) and sometimes serpiginous membrane.
Figure 7 (RIGHT): A detached retina may take on a funnel-shaped appearance.
A normal retina should be closely attached to the posterior wall of the globe such that on ultrasound there will be no distinction between the two. In the case of retinal detachment, the retinal membrane will be lifted off the posterior or lateral globe and appear as a hyperechoic (bright white) and sometimes serpiginous membrane (see Figure 6). Because of its firm attachment to the optic disc, a detached retina may take on a funnel-shaped appearance, and you will see it tethered to the optic nerve (see Figure 7). The retina’s attachment to the optic nerve posteriorly will be preserved even in the case of a retinal detachment, which is an important detail when distinguishing it from other detachments. With patient eye movements, the membrane may undulate or wave.
Involvement of the macula, in the case of retinal detachment, is a critical piece of information to obtain. The macula contains structures specialized for high-acuity vision and is located perpendicular to the lens. Once you have obtained a clear image of the retinal detachment with the lens included in the image, draw a straight line connecting the middle of the lens to the posterior wall of the globe. The area you encounter is the macula, and if it is still attached, your consult to ophthalmology becomes emergent rather than urgent. Preventing further detachment of the macula is paramount and could be a vision-saving act.
POCUS for retinal detachment has been shown to not only be possible but also accurate and precise among emergency physicians. According to a systematic review of the literature, sensitivities range from 97 to 100 percent, and specificities range from 83 to 100 percent. In a study by Blaivas et al, all retinal detachments diagnosed by ocular ultrasound performed by emergency physicians were later confirmed by a formal, masked ophthalmology evaluation, demonstrating its high specificity.3,4,5
Tips and Tricks: Be sure to scan through the entire retina and encourage eye movement while scanning as there may be small detachments of the peripheral retina that are easily overlooked.
Pages: 1 2 3 | Single Page








One Response to “High-Yield Ocular Ultrasound Applications in the ED, Part 1”
March 25, 2019
Thomas Benzoni, DO“Contraindications to the exam include high suspicion of globe rupture.”
This is a common misunderstanding.
In fact, trauma and suspicion of ruptured globe is one of the tremendously positive indications for ultrasound.
I make here an assumption that you suspect trauma or rupture and that you know not to put pressure on the globe. But that is the great thing about U/S: more goop and stand off a bit. You’ll have 0 pressure.
Compare that to any touching the eyelid to say nothing of retracting the lid.
You’re looking for obvious rupture/non-round structure.
Let’s myth-bust and use U/S to diagnose globe rupture.