Part 1 of a 3-part series. Part 2. Part 3.
The Case
Monday, 23:00—Your first patient of the night is a 65-year-old male with “no medical problems” who reports loss of vision in his right eye for the past two days. He thought it might just “go away,” but now that it hasn’t, he has placed his vision in your hands. A quick visual acuity test reveals 20/200 in the affected eye, and your attempt at a funduscopic exam reveals what you would describe as a blur of yellow and red. You have a sense of what is going on with this patient. However, you want more objective information before you speak with the ophthalmologist.
Explore This Issue
ACEP Now: Vol 38 – No 03 – March 2019Discussion
The use of ocular ultrasonography for the evaluation of emergency patients has been well-established in the emergency medicine literature. The anatomy of the eye is very complex, but luckily, point-of-care ultrasound (POCUS) can identify the key structures. The eye is a fluid-filled structure, which makes for an easy organ to visualize. With practice, POCUS can easily be incorporated into the workup of patients with ocular complaints to avoid lengthy consultation or other diagnostic tests.
The first application of diagnostic ocular ultrasound was reported by Mundt and Hughes in 1956 when diagnosing an eye tumor. Prior to ultrasound, in vivo ocular lengths and other measurements proved difficult to obtain. However, all the measurements of an eye can now be obtained by a handheld transducer.1 Today, POCUS is beyond savvy and can essentially replace the dilated funduscopic eye exam for emergency physicians. We will review the normal eye anatomy on ultrasound, techniques for the exam, as well as some high-yield ED applications on our tour of the globe!
Anatomy
When discussing anatomy, the eye is divided into two segments: anterior and posterior. The anterior segment is composed of the cornea, iris, ciliary body, and lens, while the posterior segment contains the vitreous body, posterior layers of the eye (retina, choroid, sclera), and the optic nerve (see Figure 1).
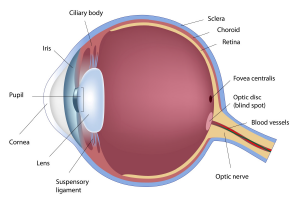
Figure 1: Anatomy of the eye.
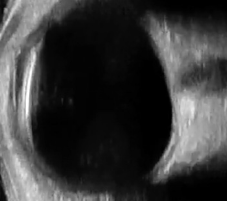
Figure 2: The fluid-filled vitreous body should appear anechoic (black) on ultrasound.
ILLUSTRATION: shutterstock.com | Photos: Nicole Yuzuk
When utilizing POCUS, the majority of your time will be spent visualizing the posterior segment. It is important to note that since the vitreous body is a fluid-filled structure, it should appear anechoic (black) on ultrasound. Hyperechoic (bright white) densities, if not artifact, should alert you to potential pathology (see Figure 2).
Pages: 1 2 3 | Single Page





One Response to “High-Yield Ocular Ultrasound Applications in the ED, Part 1”
March 25, 2019
Thomas Benzoni, DO“Contraindications to the exam include high suspicion of globe rupture.”
This is a common misunderstanding.
In fact, trauma and suspicion of ruptured globe is one of the tremendously positive indications for ultrasound.
I make here an assumption that you suspect trauma or rupture and that you know not to put pressure on the globe. But that is the great thing about U/S: more goop and stand off a bit. You’ll have 0 pressure.
Compare that to any touching the eyelid to say nothing of retracting the lid.
You’re looking for obvious rupture/non-round structure.
Let’s myth-bust and use U/S to diagnose globe rupture.