
In uncomplicated discharged AECOPD patients who are receiving antibiotics, data suggests initial empiric azithromycin, doxycycline, or trimethoprim-sulfamethoxazole are all appropriate options.3,4,7 Fluoroquinolones and amoxicillin-clavulanate were shown to be more effective than macrolides and many of the cephalosporins.3 Those who are elderly (greater than 65 years) or have severe disease (FEV1 less than 50 percent), comorbid cardiac disease, or frequent exacerbations (greater than or equal to two per year) are considered higher risk, and a course of amoxicillin-clavulanate should be considered.3,4,7 AECOPD patients with pseudomonas risk factors (prior sputum cultures growing pseudomonas, severe disease, multiple recent hospital admissions, frequent antibiotic use, or systemic steroid use) should receive pseudomonas coverage with a fluoroquinolone such as ciprofloxacin or levofloxacin.3,4,7,14,16 GOLD guidelines recommend a less than or equal to five-day course of antibiotics.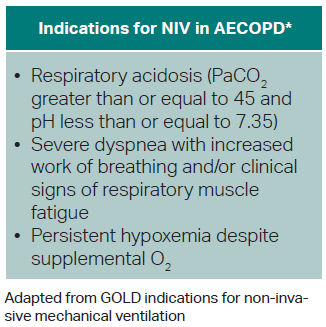
Explore This Issue
ACEP Now: Vol 43 – No 06 – June 2024Non-Invasive Positive Pressure Ventilation (NIV)
- Bilevel positive airway pressure (BPAP) preferred over continuous positive airway pressure (CPAP) for AECOPD.
- NIV decreases mortality and intubation rate and improves oxygenation, respiratory acidosis, and work of breathing.4,14
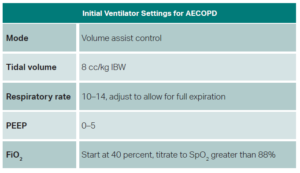
- BPAP initial settings:
- Inspiratory positive airway pressure (iPAP): 8-12 cm-H20
- Maintain iPAPs less than 20 cm-H2O to avoid gastric distension.
- Expiratory positive airway pressure (ePAP): 4-5 cm-H2O
- Titrate driving pressure (iPAP–ePAP) to adequate tidal volume and improved work of breathing via increased iPAP.11,14
- Inspiratory positive airway pressure (iPAP): 8-12 cm-H20
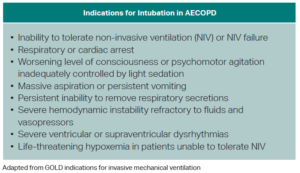
- Consider light sedation for patients who cannot tolerate NIV.4
Intubation
- No specific recommendations on which induction agents to use. Some evidence from asthma literature suggests ketamine has some bronchodilatory activity.5
- Some evidence suggests using larger diameter endotracheal tubes to avoid increasing airway resistance.11
- Ventilator settings should be targeted toward avoiding auto-PEEP and permissive hypercapnia.15
Disposition
Discharge
Generally, patients with mild to moderate symptoms on presentation, good response to ED management, no new or increased supplemental oxygen requirement, and no desaturation with ambulation can be considered for discharge. It’s good practice to address several areas of outpatient management prior to discharge to help prevent recurrence of exacerbations and ED bouncebacks: Inhaler technique should be assessed; the patient’s current maintenance therapy and their understanding of this therapy should be checked to ensure the patient is using his or her medications appropriately; counseling on smoking cessation should be performed; and close follow-up should be arranged for the patient. Good discharge instructions and strict return precautions should be provided.4
Admission or Placement in Observation Unit
Patients who present with severe symptoms, show evidence of acute respiratory failure (e.g., respiratory rate greater than 24, heart rate greater than 95, use of accessory muscles, new or increased supplemental oxygen requirement, hypercapnia above baseline, altered level of consciousness), have symptoms refractory to aggressive initial medical management, have serious comorbidities, or have a lack of home support should be strongly considered for admission or at least placement in an ED observation unit if available.4
Pages: 1 2 3 4 5 | Single Page



No Responses to “Evaluating Chronic Obstructive Pulmonary Disease”