The Case
A 61-year-old healthy female presents with two hours of right-side weakness as well as slurred speech. She has a National Institutes of Health Stroke Score/Scale (NIHSS) of 10, and you are concerned about a large vessel occlusion (LVO) based on the high NIHSS as well as the presence of both an upper extremity drift and the speech abnormality. A noncontrast computed tomography (CT) scan of her head shows no evidence of a bleed. A CT angiogram plus CT perfusion demonstrate a clot in the left proximal middle cerebral artery (MCA), with a small infarcted area and a large penumbra. She is a candidate to receive endovascular therapy (EVT) based on your institution’s current guidelines, but she is also within the current window for the administration of tissue plasminogen activator (tPA).
Clinical Question
Should you give tPA while waiting for your neurointerventional team to arrive, or is EVT alone noninferior to EVT with tPA?
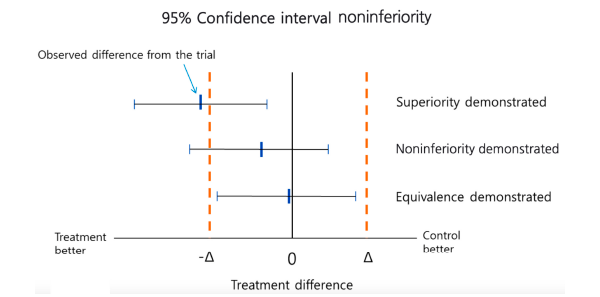
Figure 1: Testing Superiority and Equivalence/Noninferiority
Korean J Pediatr. 2012;55(11):403-407. CC BY-NC
Background: Thrombolytics as a possible treatment for acute ischemic stroke (AIS) has been discussed for decades. The famous NINDS trial led to tPA being approved for AIS within three hours of onset in those patients who met strict criteria.1 ECASS III was published in 2008 and expanded the window to 4.5 hours.2 ACEP has published guidelines on the safety and efficacy of tPA for patients with AIS. The ACEP guidelines give level B and level C recommendations.3
The controversy over the use of tPA for AIS does not seem to be going away. A recent reanalysis of ECASS III failed to show the commonly assumed benefit but confirmed the potential increase in harm of tPA. 4,5
The treatment of AIS did substantially change with the publication of the MR CLEAN trial.6 This was the first study demonstrating a benefit to endovascular treatment of a specific subset of ischemic stroke patients—specifically, those with large vessel occlusions presenting within six hours of symptom onset. MR CLEAN was followed by a number of other publications seeking to replicate and refine treatment as well as expand the window for treatment.
One major question regarding EVT treatment was whether the use of systemic thrombolytics like tPA results in better outcomes or if it simply exposes the patient to increased risks at a higher cost.
Reference: Yang P, Zhang Y, Zhang L, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. 2020;382(21):1981-1993.
Pages: 1 2 3 | Single Page





No Responses to “Endovascular Therapy With or Without tPA—What Do the Studies Say?”