A 40-year-old woman presented to our emergency department complaining of left hemiparesis and headache. She was awake and oriented, and her vitals were unremarkable except for a blood pressure of 180/100 without a history of hypertension. Past history and medications were negative. No trauma was reported. The optic nerve sheath diameter (ONSD) was measured and showed increased diameter of 0.47 cm bilaterally, demonstrating increased intracranial pressure (see Figure 1). Her level of consciousness decreased dramatically within 30 minutes, and she developed a right-sided gaze. She was intubated and underwent a brain CT showing intracranial hemorrhage in the right basal ganglia with midline shift and intraventricular hemorrhage (see Figure 2). She received a phenytoin loading dose and was taken emergently to the operating room. Fortunately, she survived with an acceptable neurologic outcome.
Explore This Issue
ACEP Now: Vol 36 – No 06 – June 2017ONSD can predict increased intracranial pressure effectively. The exact measurement can be achieved by frequent practice. Thus, this approach is being described as an operator-dependent procedure.
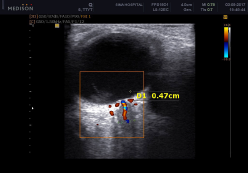
Figure 1: The optic nerve sheath diameter was measured at 0.47 cm, demonstrating an increased intracranial process in our patient.
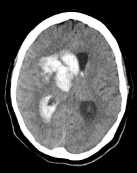
Figure 2: Brain computed tomography showed intracranial hemorrhage of the right basal ganglia as well as an intraventricular hemorrhage and a significant midline shift.
Optic Nerve Sheath Diameter
There is no doubt that ultrasonography is a valuable way to evaluate ONSD to determine intracranial pressure, considering that the brain subarachnoid space is continuous with the optic nerve sheath and the pressure should be transmitted.1–4 However, the way to measure the diameter has yet to be determined. Optic nerve color Doppler ultrasonography may clarify this measure and change what was previously approved to evaluate the ONSD. Copetti et al noted that the former measures were not compatible with the real anatomy of the optic nerve and proposed a new measurement that seems to be more reliable.1 There are two points to be considered:
- According to the route of optic nerve approaching the globe, the oblique hypoechoic shadow running medially represents the exact measure of the optic nerve (see Figure 3).
- Regarding color Doppler ultrasonography of the central retinal artery, which runs within the dural optic nerve sheath to the globe, the new image compatible with the oblique hypoechoic shadow seems more characteristic of the optic nerve.

Figure 3: Ocular ultrasound with a 12 MHz linear probe in a normal subject shows a 35 mm optic nerve diameter, identified with color Doppler.

Figure 4: Optic nerve ultrasound technique. The probe is directed slightly inferiorly and medially with the eyes closed. For better visualization, place the probe on the superior and lateral margin of the orbit.
Purpose
The evaluation of ONSD via bedside ultrasonography is beneficial in suspected cases of increased intracranial pressure transmission through the optic nerve, which leads to papilledema.
Applicability
There are common situations in which intracranial pressure assessment is necessary, but it is not possible to perform fundoscopy. Some examples include ocular media opacities such as cataract formation, hemorrhage, periorbital swelling (eg, palpebral ecchymosis in trauma patients), fixed gaze, and some infectious respiratory cases that may impose the risk of respiratory transmission.
Indications
Bedside ultrasonography can be performed in cases of suspected increased intracranial pressure (eg, traumatic brain injuries, various types of intracranial hemorrhage, space-occupying lesions, etc.).

Figure 5: The optic nerve sheath diameter should be measured 3 mm behind the retina.
Scanning Procedure
To measure the ONSD:
- Place the patient in the supine position.
- Apply sufficient amount of sterile (preferably) gel on the closed eyelid.
- Place a 6–12 MHz linear probe on the superior and lateral aspect of the upper eyelid (see Figure 4).
- Angle the probe slightly medially and caudally until the oblique hypoechoic tract of the optic nerve can be visualized with clear margins posterior to the globe. Doppler capabilities are helpful in assessing the vascularity of the optic nerve (see Figure 3).
- The diameter should be measured 3 mm behind the retina (see Figure 5).5
- For a more accurate measurement, calculate a mean of three measurements.
Pitfalls
Some reported measurements indicating an anechoic image behind the retina were probably artifacts of lamina cribrosa, the mesh-like bony structure for optic nerve fibers’ passage through the sclera, mimicking the optic nerve route, which does not follow the vascular pattern of the central retinal artery on color Doppler.1
Another pitfall is measuring the ill-defined non-clear shadow, probably the previously discussed shadow superimposed on the real ONSD. This can be prevented by carefully angulating the transducer medially and caudally to visualize the oblique ONSD with clear margins.
ONSD measurement with this method has yet to be determined in settings such as various races, different disease acuities, eye angulations, etc. Some researchers defined various measures for the ONSD. The median normal and elevated ONSD was measured at 0.42 cm (IQR 0.37–0.48 cm) in accordance with the median invasive intracranial pressure measurement that was 12 mm Hg (IQR 9–19 mmHg) and ≥ 0.48 cm for the intracranial pressures > 20 mmHg, respectively.5 The median intracranial pressure was measured by intraparenchymal external ventricular catheters. However, getting the view of the oblique hypoechoic tract of the optic nerve provides lower normal measures, around 0.35 cm, that need to be validated.
 Dr. Hossein-Nejad is assistant professor of emergency medicine at the Imam Khomeini Hospital of Tehran University of Medical Sciences in Tehran, Iran.
Dr. Hossein-Nejad is assistant professor of emergency medicine at the Imam Khomeini Hospital of Tehran University of Medical Sciences in Tehran, Iran.
 Dr. Bahreini and Dr. Rasooli are assistant professors of emergency medicine at the Sina Hospital of Tehran University of Medical Sciences.
Dr. Bahreini and Dr. Rasooli are assistant professors of emergency medicine at the Sina Hospital of Tehran University of Medical Sciences.
References
- Copetti R, Cattarossi L. Optic nerve ultrasound: artifacts and real images. Intensive Care Med. 2009;35(8):1488-1489.
- Aduayi OS, Asaleye CM, Adetiloye VA, et al. Optic nerve sonography: a noninvasive means of detecting raised intracranial pressure in a resource-limited setting. J Neurosci Rural Pract. 2015;6(4):563-567.
- Ochoa-Pérez L, Cardozo-Ocampo A. Ultrasound applications in the central nervous system for neuroanaesthesia and neurocritical care. Colombian J Anesthesiol. 2015;43(4):314-320.
- Dubourg J, Javouhey E, Geeraerts T, et al. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: a systematic review and meta-analysis. Intensive Care Med. 2011;37(7):1059-1068.
- Rajajee V, Vanaman M, Fletcher JJ, et al. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocrit Care. 2011;15(3):506-515.
Pages: 1 2 3 | Multi-Page





No Responses to “Emergency Ocular Ultrasonography to Measure Optic Nerve Sheath Diameter”