See below for a review of our four cases.
Explore This Issue
ACEP Now: Vol 36 – No 10 – October 2017I hope this helps you manage your pediatric patients with distal radius fractures. A special thanks to ACEP and Dr. Kevin Klauer for the opportunity to contribute. The goal is to highlight ED patients with commonly missed/mismanaged musculoskeletal injuries and offer strategies to help on your next shift. Comments on this column and suggestions for future ones are most welcome.
 Dr. Sayal is a staff physician in the emergency department and fracture clinic at North York General Hospital in Toronto, Ontario; creator and director of CASTED ‚Hands-On‘ Orthopedic Courses; and associate professor in the department of family and community medicine at the University of Toronto.
Dr. Sayal is a staff physician in the emergency department and fracture clinic at North York General Hospital in Toronto, Ontario; creator and director of CASTED ‚Hands-On‘ Orthopedic Courses; and associate professor in the department of family and community medicine at the University of Toronto.
Cases 1 and 3: Subtle transverse (complete or bicortical) fractures that require molding in flexion and close follow-up.
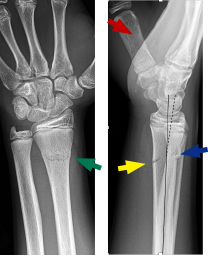 Patient 1: 14-year-old male
Patient 1: 14-year-old male
Red arrow identifies the 1st metacarpal (thumb, volar side). Blue arrow shows the dorsal buckle, but the fracture line does extend to the volar cortex (yellow arrow).
The solid black line is along the axis of the proximal fragment of the radius and extended beyond the fracture, the dashed black line is along the axis of the distal fragment, and they are not parallel. There is mild angulation of the distal fragment dorsally.
This is not a simple dorsal buckle fracture of the distal radius. This is a transverse (complete or bicortical) fracture, which is unstable with a tendency to shift dorsally. It needs to be molded in flexion.
Of note, on the posteroanterior view, the green arrow also shows the fracture across the distal radius.
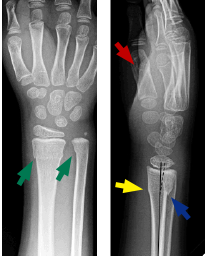 Patient 3: 7-year-old male
Patient 3: 7-year-old male
Red arrow identifies the 1st metacarpal (thumb, volar side). Blue arrow shows the dorsal buckle. On the volar side, the yellow arrow does not show a cortical break, but there is a minor change in angulation of the cortex, suggesting the fracture line extends to that point. The solid black line is along the axis of the proximal fragment of the radius and extended beyond the fracture, the dashed black line is along the axis of the distal fragment, and the lines are not parallel, so there is very mild angulation of the distal fragment dorsally.
This case is quite subtle, but this is not a simple dorsal buckle fracture of the distal radius. This is potentially unstable with a tendency to shift dorsally, so like Case 1, it’s best to be molded in flexion.





4 Responses to “Emergency Medicine Pearls, Pitfalls for Treatment of Pediatric Distal Radius Fractures”
November 19, 2017
Matt JaegerThanks so much! I appreciate your article very much. I often treat simple buckle fractures with a removable splint, but after reading your article I wonder if I may have done the same with a volar buckle fractures in the past. I will certainly change my practice. Thanks again.
July 30, 2018
Arun SayalThanks Matt.
There are tons of little pearls from our specialist colleagues – subtleties that help us manage us patients better.
Glad it helped.
Arun
November 19, 2017
AWHGreat article, and has absolutely changed my practice. Thank you Dr. Sayal!
July 30, 2018
Arun SayalThanks AWH!