
Civilian use of tourniquets has significantly increased in recent years because of the successful military implementation of tourniquets in Iraq and Afghanistan, as well as the 2014 Hartford Consensus and lay person programs such as the Stop the Bleed .1 Civilian mass-casualty events have seen growing use of tourniquets, and prehospital tourniquet application is becoming more common.1 Recent research has shown children as young as 8 can effectively learn tourniquet application.2
Explore This Issue
ACEP Now: October 2025 (Digital)When applied properly, tourniquets are extremely effective. They are strongly associated with survival in combat and may provide up to a sixfold survival benefit in prehospital civilian populations.1,3 However, as prehospital tourniquets become more ubiquitous, emergency physicians should be aware of the potential for associated complications.
Potential Complications
The U.S. military campaigns in Iraq and Afghanistan featured some of the most efficient medical evacuation (medevac) systems in the history of warfare. Evacuated soldiers with penetrating injury had a median tourniquet application duration of only 60 minutes.4 In other theaters, such as the Sahelian strip in Africa, which featured antiterrorism operations across five countries and five million square kilometers, medevac systems were far more strained, and tourniquet duration for injured soldiers frequently exceeded two hours, resulting in significant complications.4 The Russo-Ukrainian War is an even more extreme example, with a mean medevac time of as long as 21 hours.5 These conflicts have shown the dangers of Prolonged Tourniquet Application Syndrome (PTAS).
PTAS is also likely to become more common in the civilian setting. Although medically indicated tourniquets are lifesaving, civilian settings have an incidence of not medically indicated tourniquets that ranges from 10.5 percent to 100 percent in various case studies.5
Tourniquets that have been in place for longer than two hours carry significant risks, including local and systemic reperfusion effects when removed, compartment syndrome, and rhabdomyolysis.3 Tourniquet use also induces a hypercoagulable state and increases the risk for thromboembolism.6 The release of antioxidants from reperfusion may have a wide range of cascading effects, with potential for hepatic, renal, and pulmonary dysfunction after tourniquet removal.6 Given this, the two-hour mark should be considered critical for emergency physicians.3
Tourniquets in the ED
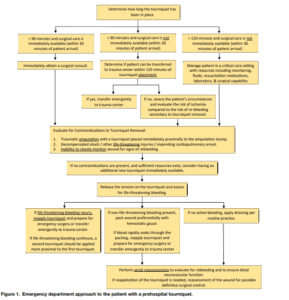
FIGURE 1: ED management of prehospital tourniquet.3 Click to enlarge. (Reprinted from The Journal of Emergency Medicine, 60:1, Levy MJ et al., “Removal of the Prehospital Tourniquet in the Emergency Department, Copyright 2021, with permission from Elsevier.)
Upon arrival to the emergency department (ED), any patient with a prehospital tourniquet should have the time of their tourniquet application determined. If a specific time is not known, it should be assumed to be at the same time that EMS arrived at the scene of the accident.3 It should also be determined if the tourniquet is medically necessary—not medically indicated tourniquets are often applied in the prehospital setting.5
As shown in Figure 1, the timing of the tourniquet application determines the next steps. If it has been less than 90 minutes and surgery is available, an immediate surgical consult should be placed to minimize ischemic injury to the patient. If it has been longer than 120 minutes, the patient should be assessed for any contraindications to tourniquet removal—including decompensated shock, inability to directly monitor the patient for at least one hour after tourniquet removal, or a traumatic amputation with the tourniquet within several inches of the amputation stump. If there are no contraindications, the tourniquet should be removed in a critical care setting with monitoring, fluids, resuscitation meds, and surgical services available.3
If less than 90 minutes and surgery is not available, the patient should be transferred to a trauma center within 120 minutes of the initial tourniquet placement. If this is also not possible, the patient should be assessed for risk for PTAS versus the risk for re-bleeding secondary to tourniquet removal, considering the contraindications listed above.3 If there are no contraindications, tourniquet removal may be attempted.
When removing the initial tourniquet, a new tourniquet should be available. The initial tourniquet should have its tension eased—if any life-threatening bleeding starts, it should be retightened, with the second tourniquet also applied within several inches of the wound, noting the time. If there is a non–life-threatening bleed, hemostatic gauze may be applied with manual pressure for three to five minutes and secured with pressure dressing.
If the blood rapidly soaks through the gauze, the original tourniquet should be tightened. If this bleed continues, the second tourniquet should be applied. If there is no bleeding, or bleeding is controlled, the patient should be closely observed for a minimum of one hour to ensure there is no rebleeding. In all these cases, the original tourniquet should be kept loose on the limb in case it is needed for any emergent rebleeding.3 In all cases, close wound monitoring is imperative.4
 Dr. Turner originally trained at the Medical University of South Carolina, and is an emergency medicine resident at Hershey Medical Center in Hershey, Pa.
Dr. Turner originally trained at the Medical University of South Carolina, and is an emergency medicine resident at Hershey Medical Center in Hershey, Pa.
References
- Smith AA, Ochoa JE, Wong S, et al. Prehospital tourniquet use in penetrating extremity trauma: decreased blood transfusions and limb complications. J Trauma Acute Care Surg. 2019;;86(1):43-51.
- Chang CD, Bosson N, Gausche-Hill M, et al. Assessing hemorrhage control and tourniquet skills in school-aged children. J Am Coll Emerg Physicians Open. 2025;6(3):100078.
- Levy MJ, Pasley J, Remick KN, et al. Removal of the prehospital tourniquet in the emergency department. J Emerg Med. 2021;60(1):98-102.
- Sabate-Ferris A, Pfister G, Boddaert G, et al. Prolonged tactical tourniquet application for extremity combat injuries during war against terrorism in the Sahelian strip. Eur JTrauma Emerg Surg. 2022;48(5):3847-3854.
- Butler F, Holcomb JB, Dorlac W, et al. Who needs a tourniquet? And who does not? Lessons learned from a review of tourniquet use in the Russo-Ukrainian war. J Trauma Acute Care Surg. 2024;97(2S):S45-54.
- Leurcharusmee P, Sawaddiruk P, Punjasawadwong Y, et al. The possible pathophysiological outcomes and mechanisms of tourniquet‐induced ischemia‐reperfusion injury during total knee arthroplasty. Oxid Med Cell Longev. 2018;2018(1):8087598.
Pages: 1 2 3 | Multi-Page





No Responses to “Emergency Department Management of Prehospital Tourniquets”