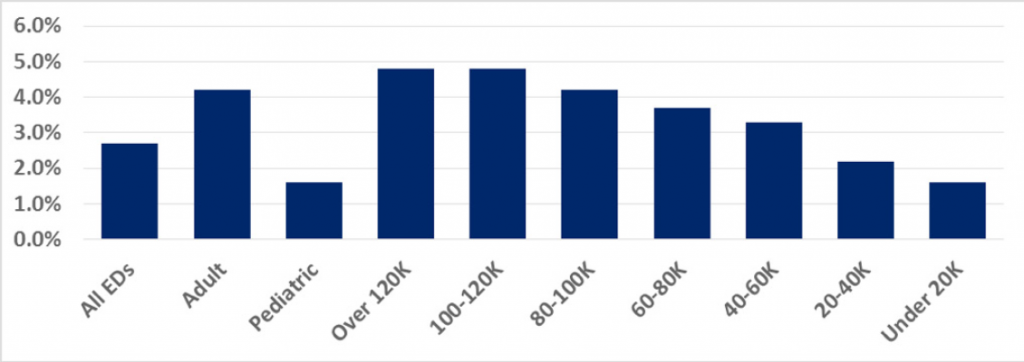
In 2017, the LBTC rate was 2.7 percent across all emergency departments, but it varied significantly across the various cohorts that represent different types of emergency departments and different ED volumes. The LBTC rate by cohort appears in Figure 2.
Explore This Issue
ACEP Now: Vol 37 – No 11 – November 2018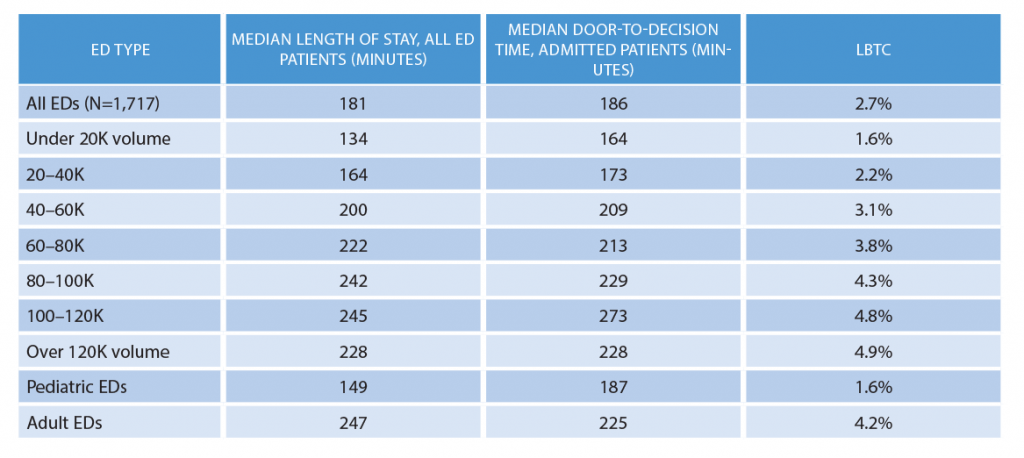
(click for larger image) Table 2: 2017 Emergency Department Benchmarking Alliance Data Survey Results
Table 2 shows the EDBA time intervals and LBTC rate. That data suggests a correlation between processing all patients, the door-to-decision time for admitted patients, and overall walkaway rates. And it clearly reflects the stresses on ED operations when volume and patient acuity increase.
The overall complexity of processing patients who ultimately are admitted is reflected in the amount of time it takes across all cohorts to arrive at the decision to admit. Even in the smallest emergency departments, the median time to that decision was 164 minutes. The other ED cohorts reported a time range of roughly 180–228 minutes, except for the group of emergency departments in the 100,000–120,000 volume range, where the time to decision averages 273 minutes. Long time intervals to decision to admit or discharge are associated with higher LBTC rates.
Conclusions
We can see emergency physicians have an opportunity to reduce walkaway rates by improving decision timing. Many emergency departments have reduced door-to-provider time, but we also need a timely effort to perform diagnostic testing and get the results to the responsible emergency physician, initiate any necessary treatment and evaluate the results, conduct necessary conversations with primary care or other consulting physicians, and complete a review of pertinent medical records. All of those items combined will give the emergency physician an opportunity to make a quality disposition decision and initiate transition of care.
Decision to admit by an emergency physician begins a cascade of events that should end in a timely movement of the patient to the inpatient unit. A boarding time discussion took place in a 2016 ACEP Now article, but unfortunately the EDBA boarding time numbers in 2016 and 2017 remained consistent at about 117 minutes.4
Despite ED volume and acuity increases that challenge ED providers, improved operations have been evident in many emergency departments. However, the LBTC rates relate to ED efficiency and processing, and improving those areas requires coordinated utilization of staff, equipment, processes, and documentation.
Pages: 1 2 3 | Single Page





One Response to “Emergency Department Inefficiency Drives Poor Quality”
December 2, 2018
Rob Beatty, MD FACEPGood article. In the time frame reported, there has been a major push for EMR conversion due to meaningful use requirements. Some of those EMRs impact house-wide processes as a whole, which could cause significant increases in lab/radiology turnaround time, and add additional human steps to workflow that were not in practice previously. Have you considered evaluating these additional data points and seeing how they fit into your analysis?