The Case
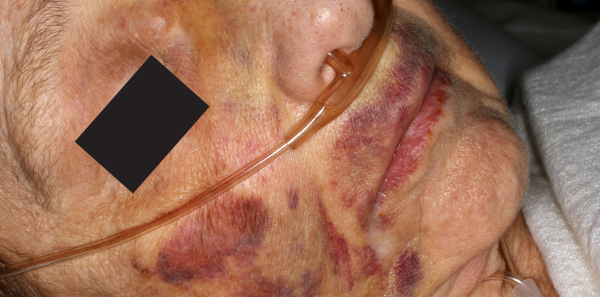
A 74-year-old female nursing home resident with moderate dementia presents with her daughter for evaluation of rash to the mother’s face and arms (see Figure 1). The daughter has not seen her mother for several weeks due to COVID-19 visitation restrictions. The nursing home cannot explain how the resident got the bruises. There were no reports of a fall. The last time the daughter video-chatted with her mom was about two weeks ago. The daughter also says her mom seems quieter and more withdrawn than usual. Her mother seemed fearful of the male medics who transported her to the emergency department.
Explore This Issue
ACEP Now: Vol 39 – No 09 – September 2020Discussion
The Centers for Disease Control and Prevention defines elder abuse as “an intentional act or failure to act that causes or creates a risk of harm to an older adult. An older adult is someone age 60 or older. The abuse often occurs at the hands of a caregiver or a person the elder trusts.”1 Legal definitions vary from state to state. Elder abuse can be further divided into neglect (the most common form of abuse), physical abuse, sexual abuse, financial abuse, and emotional/psychological abuse.
Elder abuse is a serious problem and a public health emergency. It is estimated that one in 10 people older than 60 who live at home are abused.2,3 This is likely a substantial underestimate as studies often only look at ED visits and not other sites of care like primary care offices and clinics. A high number of cases are thought to go unreported because patients do not have someone who can advocate on their behalf.
There are numerous physical and emotional effects of elder abuse. Physical injuries can be minor or severe and can cause lasting or permanent disabilities. These injuries can lead to premature death and worsen existing health problems. There are also immediate and long-term emotional effects. Victims are often fearful and anxious. They may have problems trusting others and are wary around them.
There are several identified risk and protective factors for elder abuse perpetration. Risk factors can be divided as individual, relationship, institutional, and societal. Individual factors include: current diagnosis of mental illness, alcohol or drug abuse, high levels of hostility, poor or inadequate preparation or training for caregiving responsibilities, early age assumption of caregiving responsibilities, inadequate coping skills, and exposure to abuse as a child. Relationship factors include: high financial and emotional dependence upon a vulnerable elder, past experience of disruptive behavior, lack of social support, and lack of formal support. Institutional factors include: unsympathetic or negative attitudes toward residents, chronic staffing problems, and lack of administrative oversight, staff burnout, and stressful working conditions. Societal factors include a culture where there is high tolerance and acceptance of aggressive behavior; health care personnel, guardians, and other agents are given greater freedom in routine care and decision making; family members are expected to care for elders without seeking help from others; persons are encouraged to endure suffering or remain silent regarding any pain and suffering; and negative beliefs about aging and elders exist.4,5 It should be noted, however, that the presence of risk factors does not necessarily mean an elder will be abused.
Protective factors against elder abuse have not been as extensively studied as risk factors. Institutional protective factors include effective monitoring systems,, solid institutional policies and procedures regarding patient care, regular training on elder abuse and neglect for employees; education and clear guidance on durable power of attorney and how it is to be used; and regular visits by family members, volunteers, and social workers. The other factors are based on strong sense of community; respect for elders; and healthy, strong relationships.
In additional to the protective factors and elder abuse prevention strategies, one of the key factors in stopping abuse is early recognition by health care workers. Elders should be screened for abuse using any of several validated tools. In the emergency department, there are several red flags that should alert the care team to the possibility that an elder is being abused. These include a lack of basic hygiene, food, medical aids, and clean and appropriate clothing; a person with dementia left unsupervised; a bed-bound person left without care; untreated or unusual pressure sores/ulcers; a caregiver who isolates the elder; a caregiver who is verbally aggressive or demeaning to the elder; inadequately explained fractures, bruises, welts, cuts, sores, or burns; a delay in seeking care for obvious injuries or conditions; unexplained sexually transmitted infections; and behavioral changes.6
Health care workers in most states are mandated reporters of elder abuse and should alert the proper authorities and adult protective services when abuse or neglect is suspected. Patients may require additional workup to determine abuse from progression of chronic diseases, as well as admission to the hospital for the patient’s protection.
Case Outcome
The emergency physician was concerned that the rash was actually bruising and suspected elder abuse. Labs, X-rays, and CT scans were negative. A forensic nurse examiner was consulted. On exam, in addition to the bruises, there was evidence of genital injury and vaginal discharge, which subsequently tested positive for chlamydia. Based on the concern for abuse, police and adult protective services were consulted. An investigation identified a dietary worker at the nursing home as the perpetrator.
Dr. Rozzi is an emergency physician, director of the Forensic Examiner Team at WellSpan York Hospital in York, Pennsylvania, and chair of the Forensic Section of ACEP.
Dr. Riviello is chair and professor of emergency medicine at the University of Texas Health Science Center at San Antonio.
References
- Hall JE, Karch DL, Crosby A. Elder Abuse Surveillance: Uniform definitions and recommended core data elements. Version 1.0. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. CNPEA website. Accessed July 27, 2020.
- Acierno R, Hernandez MA, Amstadter AB, et. al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292-297.
- Logan JE, Haileyesus T, Ertl A, et al. Nonfatal assaults and homicides among adults aged ≥60 years – United States, 2002-2016. MMWR Morb Mortal Wkly Rep. 2019;68(13):297-302.
- Wilkins N, Tsao B, Hertz M, et al. Connecting the dots: an overview of the links among multiple forms of violence. Centers for Disease Control and Prevention website. Accessed July 27, 2020.
- Abuse of the elderly. In: Krug EG, Dahlberg LL, Mercy JA, et al, eds. World report on violence and health. 2002:125-145. World Health Organization website. Accessed July 27, 2020.
- Red flags for elder abuse. Center of Excellence on Elder Abuse & Neglect website. University of California Irvine, Irvine, CA;. Accessed July 27, 2020.
Pages: 1 2 | Multi-Page





No Responses to “Early Recognition in the Emergency Dept Is Key to Stopping Elder Abuse”