Case Outcome
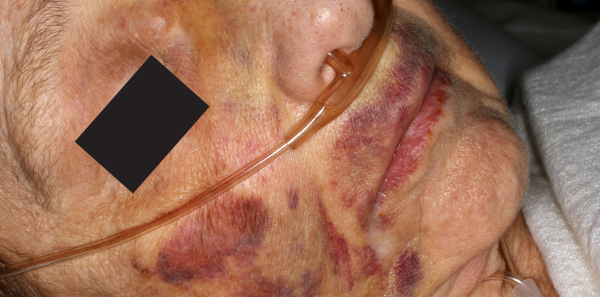
The emergency physician was concerned that the rash was actually bruising and suspected elder abuse. Labs, X-rays, and CT scans were negative. A forensic nurse examiner was consulted. On exam, in addition to the bruises, there was evidence of genital injury and vaginal discharge, which subsequently tested positive for chlamydia. Based on the concern for abuse, police and adult protective services were consulted. An investigation identified a dietary worker at the nursing home as the perpetrator.
Explore This Issue
ACEP Now: Vol 39 – No 09 – September 2020Dr. Rozzi is an emergency physician, director of the Forensic Examiner Team at WellSpan York Hospital in York, Pennsylvania, and chair of the Forensic Section of ACEP.
Dr. Riviello is chair and professor of emergency medicine at the University of Texas Health Science Center at San Antonio.
References
- Hall JE, Karch DL, Crosby A. Elder Abuse Surveillance: Uniform definitions and recommended core data elements. Version 1.0. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. CNPEA website. Accessed July 27, 2020.
- Acierno R, Hernandez MA, Amstadter AB, et. al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292-297.
- Logan JE, Haileyesus T, Ertl A, et al. Nonfatal assaults and homicides among adults aged ≥60 years – United States, 2002-2016. MMWR Morb Mortal Wkly Rep. 2019;68(13):297-302.
- Wilkins N, Tsao B, Hertz M, et al. Connecting the dots: an overview of the links among multiple forms of violence. Centers for Disease Control and Prevention website. Accessed July 27, 2020.
- Abuse of the elderly. In: Krug EG, Dahlberg LL, Mercy JA, et al, eds. World report on violence and health. 2002:125-145. World Health Organization website. Accessed July 27, 2020.
- Red flags for elder abuse. Center of Excellence on Elder Abuse & Neglect website. University of California Irvine, Irvine, CA;. Accessed July 27, 2020.
Pages: 1 2 | Single Page





No Responses to “Early Recognition in the Emergency Dept Is Key to Stopping Elder Abuse”