Explore This Issue
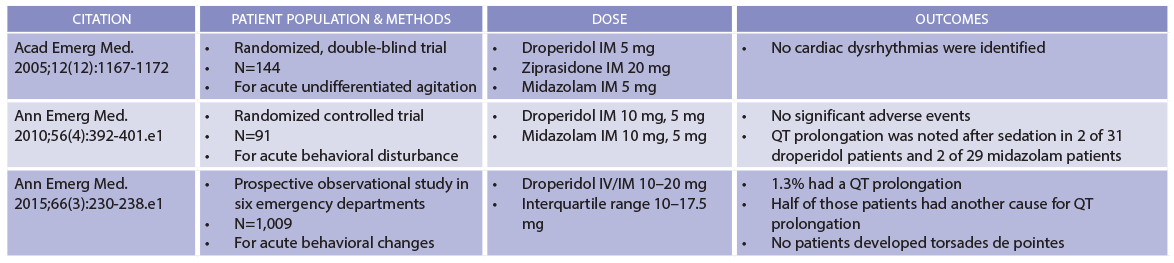
ACEP Now: Vol 38 – No 09 – September 2019(click for larger image) Table 1: Droperidol Safety Data
Compiled by Brigham and Women’s Hospital Drug Safety Committee.
Second, droperidol is a smarter choice for sedation than lorazepam. Clinical trials have demonstrated that agitated patients need additional doses of lorazepam five times more frequently than those receiving droperidol.5 In other words, while a patient may need only a single 5 mg dose of droperidol, a comparable patient may need 2 mg lorazepam—again and again and again and again. The issue here is one of pharmacodynamics. Physicians often recognize that lorazepam has a relatively short plasma half-life, but control of agitation is a pharmacodynamic effect. Lorazepam has slower central nervous system (CNS) penetrance, so sedation is delayed. Because achieving sedation takes longer, clinicians often give additional doses of lorazepam before the previous dose has fully taken effect. The serial administration of lorazepam is a real problem. Sedation following parenteral lorazepam typically lasts six to eight hours, but sedation following repeat dosing can persist even longer, sometimes up to 24 hours.
Droperidol avoids the oversedation commonly seen in lorazepam (and other benzodiazepine) therapy. Droperidol, with its brisk CNS penetrance, sedates faster, so clinicians can “tune” the degree of behavioral control to a particular clinical scenario, eliminating frequently incorrect stacked dosing of benzodiazepines. This alone may help avoid an unnecessary hospitalization of a patient who—after receiving multiple doses of lorazepam—“just won’t wake up.” Using droperidol instead has the potential to decrease lengths of stay for intoxicated patients who have temporarily become a belligerent threat to themselves and others in the emergency department.
Third, droperidol is a better choice for controlling agitation than haloperidol, which became the mainstay choice over the last 20 years during which droperidol was largely unavailable here. While haloperidol is a superb antipsychotic, it is a lousy sedative. That’s why a sedative (such as lorazepam) is often needed for behavioral control—we’ve known since at least the 1980s that haloperidol alone simply doesn’t cut it—thus the “5 and 2” strategy that has become the reflexive approach for controlling the agitated ED patient. Single drug therapy is often safer than polypharmacy, an aphorism supported by studies pitting droperidol versus haloperidol plus lorazepam. Lorazepam tends to oversedate patients, often for long periods of time. For those of us old enough to be familiar with droperidol’s wondrous ability to rapidly control agitation without snockering the patient for hours, we remember that its use translated into simpler dispositions; formerly agitated drunks essentially “went down” but could be easily awakened and discharged by shift’s end.
Finally—and this is important for emergency physicians—there is no need for an ECG prior to droperidol administration at common ED doses. Continuous cardiovascular monitoring to detect torsades is not mandated and usually unnecessary. This is based upon the knowledge that any observed QT prolongation following droperidol administration is both uncommon and, even if present, almost always clinically insignificant. Interestingly, data from some studies seem to suggest that lorazepam is actually more likely to be associated with QT prolongation, although the mechanism for this is not clear and it certainly did not lead to cardiac dysrhythmias.3
Pages: 1 2 3 | Single Page





3 Responses to “Droperidol Is Back (and Here’s What You Need to Know)”
October 19, 2019
Marguerite WrightExcellent article. It would be interesting to follow the use of this drug as it becomes more widely used in the acute clinical setting.
November 21, 2019
Marc Hoffman,MDDr. Boyer,
We are currently trying to get droperidol back on formulary at Mercy Hospital in Portland, for use in the ED. At Brigham, it seems you are not checking the QTc, am I correct? Is there a subset of patients you check the QTc on once they are more sedate?
December 28, 2019
M Bruce Parker MD FACEPI have presented this [& other] articles
to the EDs where I work, to no avail.
Will we wait another 17 years for a new generation of managers to not remember thinking inside this box? When there is no money to be made, progress is slow.