The patient’s family filed a lawsuit against both emergency physicians, both hospitals, and the surgeon.
At deposition, the attorneys asked the second emergency physician if he felt he released an unstable patient in light of her last documented heart rate of 142 bpm. He responded, “She was not unstable in my opinion. She was alert, talkative, pleasant. Her pain had been relieved. She had a blood pressure of 130/80. She had a good sat. I wouldn’t call her unstable.”
In addition to a medical malpractice claim, the lawsuit specified an EMTALA violation as well.
The EMTALA claims were dismissed by the judge because the second emergency physician never identified an emergency medical condition. (Note: Failing to detect an emergency condition is an acceptable defense against an EMTALA violation, though clearly not against a malpractice claim.)
The medical malpractice claims were settled out of court. The exact details are unknown, but a seven-figure settlement would be typical.
Discussion
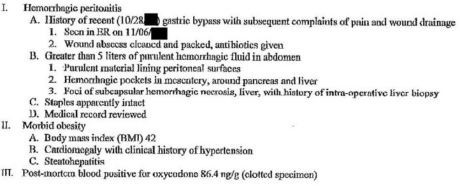
This case provides an example of the dangers of discharging patients with tachycardia. Discharging a patient with tachycardia is not universally contraindicated in cases where the tachycardia is relatively mild and the patient has a credible low-risk explanation. However, this patient met neither criteria. A heart rate of 142 bpm (with an upward trend) in the setting of recent gastric bypass was a recipe for disaster.
The defendant’s claim that the patient was not unstable with a heart rate of 142 bpm was misguided.
On the second visit, there was documentation that the patient had not filled her prescriptions. While it is frustrating when patients return to the emergency department without following the instructions they were given at the time of the previous discharge, it doesn’t mean their bounceback visit can be dismissed. In fact, a return visit may be the last chance we have to prevent a catastrophic outcome.
The second emergency physician clearly did not want to do any workup or bother the surgeon again. Instead of making one more phone call to transfer the patient, he ended up dragging his partner and the surgeon into a multiyear litigation process. Don’t follow in the footsteps of this physician and miss your final opportunity to reverse course and save a life.
 Dr. Funk is a practicing emergency medicine physician in Springfield, Missouri, and owner of Med Mal Reviewer, LLC. He writes about medical malpractice at www.medmalreviewer.com.
Dr. Funk is a practicing emergency medicine physician in Springfield, Missouri, and owner of Med Mal Reviewer, LLC. He writes about medical malpractice at www.medmalreviewer.com.
Pages: 1 2 3 | Single Page




No Responses to “Don’t Be Shy When Evaluating Patients Who Return to the ED”