A 45-year-old female presented to the emergency department approximately three hours after a suspected intentional multidrug overdose, which included extended-release bupropion and amitriptyline among several other medications. On arrival, the patient exhibited tonic-clonic seizures and required emergent endotracheal intubation. Her vital signs were notable for profound hypotension (BP 51/35 mmHg) and relative bradycardia (HR 68 bpm).
Explore This Issue
ACEP Now: November 2025An initial ECG revealed a widened QRS (136 ms) and prolonged QTc (521 ms). Vasopressor support with norepinephrine was initiated, and sodium bicarbonate therapy was started and titrated to a serum pH of 7.50-7.55, resulting in QRS narrowing. This initial management stabilized her hemodynamics, but despite aggressive supportive care, her neurologic exam showed absent brainstem reflexes. These findings raised concern for irreversible anoxic brain injury versus pharmacologic brain death due to drug toxicity.
Diagnosis and Management
This case represents a rare and severe presentation of polypharmacy overdose with a focus on massive bupropion and amitriptyline ingestion leading to seizures, cardiogenic shock, and loss of brainstem reflexes — ultimately exacerbated and prolonged due to a gastric pharmacobezoar, which resulted in delayed and continuous absorption of the ingested medications. Toxicology screens later confirmed elevated serum bupropion (600 ng/mL) and hydroxybupropion (3000 ng/mL) levels. Amitriptyline levels were not obtained.
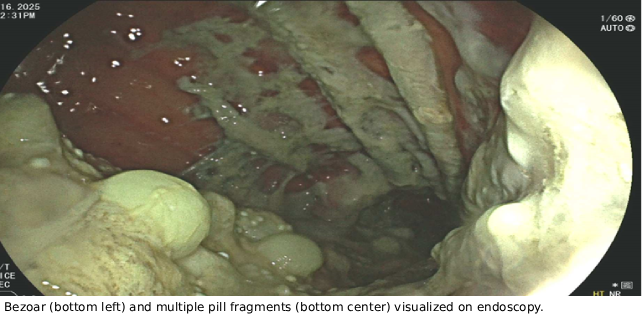
Initial management followed standard toxicologic principles: airway protection, seizure control, hemodynamic support, and QRS narrowing with sodium bicarbonate. Continuous sedation with propofol was needed for seizure suppression, and a norepinephrine infusion was necessary for blood pressure stabilization. An echocardiogram revealed preserved cardiac systolic function. Due to the persistence of neurologic dysfunction and hemodynamic lability, the patient underwent upper endoscopy 18 hours post-ingestion.
Upper endoscopy confirmed a bezoar composed of pill fragments and gastric contents. Whole bowel irrigation (WBI) with polyethylene glycol-electrolyte solution (PEG-ELS) at 2 L/hr and activated charcoal were initiated. This intervention led to a transient increase in QRS widening (174 ms) due to increased mobilization and absorption, which was treated with additional sodium bicarbonate to overcome the known cardiotoxic effects of both amitriptyline and bupropion. The absence of serum concentrations at this time limited confirmation but strongly supported ongoing absorption of both medications.
Discussion
Bupropion and amitriptyline both exert significant toxicologic effects in overdose due to their impact on neurotransmitter systems and cardiac conduction. Bupropion inhibits the reuptake of dopamine and norepinephrine, resulting in excessive catecholaminergic stimulation. Both agents block cardiac fast sodium channels and potassium channels, which can cause QRS and QTc prolongation. Additionally, tricyclic antidepressants like amitriptyline inhibit gap junctions between cardiomyocytes, disrupting electrical conduction, and potentially leading to arrhythmias or systolic dysfunction. These mechanisms collectively offer explanations for the observed seizures, cardiac conduction abnormalities, and central nervous system (CNS) depression in this patient.
The patient’s clinical course was further complicated by prolonged unresponsiveness and absent corneal, pupillary, cough, and gag reflexes — features concerning for possible brain death. Continuous electroencephalography (EEG) showed a spindle coma pattern with burst suppression. However, given the known delayed clearance and CNS effects of bupropion and tricyclic antidepressants, premature neuro-prognostication was avoided. In our patient, levetiracetam was included in the antiepileptic regimen. Although continuous seizure activity was not observed on EEG, levetiracetam was used in part to address suspected postictal cortical irritability and to prevent progression of nonepileptic myoclonus — a recognized manifestation of bupropion toxicity and a rare manifestation of amitriptyline toxicity. While benzodiazepines remain first-line, adjunctive agents like levetiracetam may be helpful in managing neuroexcitation syndromes.
On hospital day nine, the patient was successfully extubated. She regained full brainstem function and was awake and responsive, albeit agitated. The patient required re-intubation due to severe hypoxia and agitation. She later required tracheostomy due to persistent airway swelling, which was completed by general surgery on hospital day 17. The patient was discharged to an inpatient psychiatric unit on hospital day 31 for further care, ultimately going home 39 days after initial ingestion with limited memory of these events but otherwise fully neurologically intact.
This case highlights the potentially devastating complications of sustained-release antidepressant overdose, including pharmacobezoar formation, cardiotoxicity, and prolonged CNS suppression. It highlights the need to maintain clinical suspicion for bezoars when toxicity is prolonged, especially when extended-release formulations are involved. Upper endoscopy can play a diagnostic role when radiographic or clinical suspicion is high. Interventions like whole bowel irrigation may be therapeutic but require monitoring for drug “dumping” and resultant clinical worsening.
Teaching Points
- Consider pharmacobezoar in prolonged or worsening toxicity, especially with sustained-release, anticholinergic and cardiotoxic agents.
- Avoid early neuro-prognostication in toxicologic comas, particularly with agents known to mimic brain death.
- Whole bowel irrigation can be effective but may transiently increase drug absorption and toxicity — monitor closely during administration.
 Dr. Duheric is a third-year emergency medicine resident at Corewell Health Lakeland. She did her medical school training at the Chicago College of Osteopathic Medicine and in her free time enjoys reading, going to concerts and traveling with her husband and dog.
Dr. Duheric is a third-year emergency medicine resident at Corewell Health Lakeland. She did her medical school training at the Chicago College of Osteopathic Medicine and in her free time enjoys reading, going to concerts and traveling with her husband and dog.
References
- Amitriptyline. Reactions Weekly. 1647, 25 (2017). https://doi.org/10.1007/s40278-017-28718-3
- Inoue F, Okazaki Y, Huh K, et al. Pharmacobezoar Associated Prolonged Clinical Course in a Patient with Immediate Release Quetiapine Overdose. J Med Toxicol.. 2024;20(4),430-433. https://doi.org/10.1007/s13181-024-01029-6
- Murphy L, Wolfer H, Hendrickson RG. Toxicologic Confounders of Brain Death Determination: A Narrative Review. Neurocrit Care. 2021;34(3), 1072-1089. https://doi.org/10.1007/s12028-020-01114-y
- Pelletier JN, Ie SR, Stromberg PE, et al. Back from the Dead: A Case of Bupropion Overdose Mimicking Brain Death. J Clin Toxicol. 2020;10(4), e1000447. https://doi.org/10.35248/2161-0495.20.10.447
- Simon M, Kaplan S, Muschler K, et al. The role of QRS complex prolongation in predicting severe toxicity in single-xenobiotic overdose. Clin Toxicol. 2024;62(1), 32–38. https://doi.org/10.1080/15563650.2024.2307356
- Stranges D, Lucerna A, Espinosa J., et al. A Lazarus effect: A case report of bupropion overdose mimicking brain death. WJEM. 2018; 9(1), 67-69. https://doi.org/10.5847/wjem.j.1920-8642.2018.01.011
- Xiang XM, Phillips D J. Nonepileptic myoclonus following bupropion overdose. ClinPediatr 2018;57(9),1100-1102. https://doi.org/10.1177/0009922817737082
Pages: 1 2 3 | Multi-Page





No Responses to “Case Report: Massive Amitriptyline and Bupropion Ingestion”