This is the second in a multi-part ACEP Now series focused on mental health emergencies. Last month’s article focused on ACEP’s efforts and resources to support EDs and patients with psychiatric emergencies. Future articles will highlight solutions and success stories. This month, we are discussing the medical management of patients with mild to moderate agitation.
Explore This Issue
ACEP Now: Vol 42 – No 07 – July 2023Emergency departments (EDs) focus on rapid initiation of medical treatment. Patients with sepsis get antibiotics. Patients with opiate overdose get naloxone. Patients in DKA get insulin. And yet, when many patients arrive with a mental health crisis, they get nothing—until they escalate, at which point they often get too much and remain over-sedated for hours. Just as for patients experiencing other emergencies, ED physicians should rapidly initiate appropriate medical treatment for patients experiencing mental health crises, before they decompensate.
Calming Measures
Sometimes ED physicians are reluctant to initiate calming treatment in lower acuity patients, preferring to wait until more aggressive sedation is absolutely necessary. They might have been instructed that early calming measures lead to an inaccurate evaluation of the patient by a mental health professional or worry about over-sedating the patient. However, rapid initiation of treatment is actually patient-centered care that can both lead to better outcomes and limit ED boarding. Mental health evaluation teams can rely on documentation and interviews to understand a patient’s initial agitation level. It is also equally important for mental health evaluators to understand how patients respond to calming medication, as that can help guide inpatient versus outpatient treatment decisions.
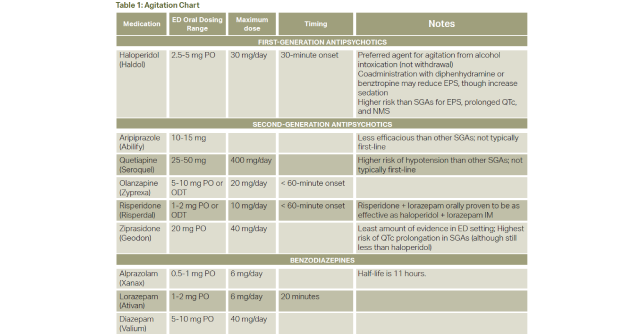
This article focuses on calming medication in patients with mild to moderate agitation. The article also will not address severe agitation, which is already well covered elsewhere and is the topic of an ACEP clinical policy currently in development.1–3
When to Consider Calming Treatments
Calming treatment should be considered immediately upon arrival for patients who are experiencing agitation or anxiety, even if the symptoms are not severe.4 The first step is to establish a therapeutic alliance and engage in verbal de-escalation.5 ED physicians should use a calm, non-confrontational tone, respect the patient’s personal space, set polite but firm boundaries for behavior, and offer choices where appropriate. Sometimes investing an extra two to five minutes—certainly a significant time commitment on a busy shift—to establish trust can limit the need to spend even more time later in the shift managing escalating behavior (or permit a much earlier disposition).
Pages: 1 2 3 4 | Single Page





One Response to “Agitation Treatment in the Emergency Department”
July 12, 2023
John SmithI appreciate the article’s emphasis on the importance of early intervention in the treatment of agitation. Agitation can quickly escalate, so it is important to intervene early to prevent a patient from becoming more aggressive or violent.