In 2021, the American College of Gastroenterology (ACG) published an update of their 2012 management guideline on upper gastrointestinal bleeding (UGIB).1,2 The updated guideline included a total of 16 recommendations, of which five are relevant to emergency medicine practice:
Explore This Issue
ACEP Now: Vol 41 – No 07 – July 2022- ACG suggests that patients presenting to the emergency department with upper gastrointestinal bleeding (UGIB) who are classified as very low risk, defined as a risk assessment score with ≤1% false negative rate for the outcome of hospital-based intervention or death (e.g., Glasgow-Blatchford score 0–1), be discharged with outpatient follow-up rather than admitted to hospital (conditional recommendation, very-low-quality evidence).
- ACG suggests a restrictive policy of red blood cell transfusion with a threshold for transfusion at a hemoglobin of 7 g/dL for patients with UGIB (conditional recommendation, low-quality evidence).
- ACG suggests an infusion of erythromycin before endoscopy in patients with UGIB (conditional recommendation, very-low-quality evidence).
- ACG could not reach a recommendation for or against pre-endoscopic proton pump inhibitor (PPI) therapy for patients with UGIB.
- ACG suggests that patients admitted to or under observation in hospital for UGIB undergo endoscopy within 24 hours of presentation (conditional recommendation, very-low-quality evidence).
Of these five recommendations there were three notable changes from the 2012 guideline.
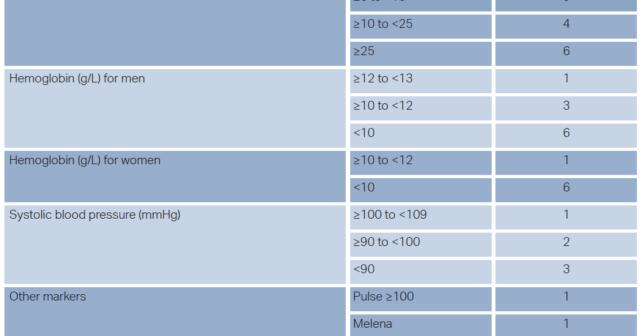
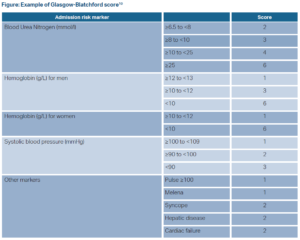
First, in risk stratifying patients, the 2021 recommendation now incorporates risk assessment scores in determining which patients are safe for discharge from the emergency department. ACG defined an appropriate risk assessment score as one with a sensitivity of ≥ 99% (i.e., a false negative rate ≤ 1%). Comparing meta-analyses, systemic reviews, and individual test accuracy studies of the Glasgow-Blatchford score, AIMS65 score, preendoscopy Rockwell score, and a published machine learning model,only the Glasgow-Blatchford and the machine learning model consistently met this standard.3 Therefore, the Glasgow-Blatchford score is the only readily available risk assessment score appropriate for use (sensitivity 0.99). Additionally, ACG expanded the number of patients the recommendation reaches suggesting that patients with a score of either 0 or 1 on the Glasgow-Blatchford score have a sufficiently small false negative rate and can be safely discharged from the emergency department (see Figure 1).
The second change revolved around the lack of recommendation for, or against, preendoscopic PPI use for patients with UGIB. The 2012 management guideline stated that preendoscopy PPI use may be considered whereas no recommendation could be reached for this 2021 guideline. This change was based on several factors. One was additional evidence available since the 2012 management guideline and subsequent meta-analysis by ACG which showed no difference in further bleeding or mortality with pre-endoscopy PPI (the benefit of PPI post-endoscopy is well known and accepted). Additionally, evolving consensus on the structure of guideline recommendations focuses on recommending specific actions. With this evolution, the ACG’s 2012 statement of “pre-endoscopic intravenous PPI may be considered” no longer fits current guideline structure. The meta-analysis conducted by ACG revealed patients with pre-endoscopic PPI had lower rates of evidence of recent hemorrhage and lower rates of hemostatic treatment during endoscopy compared to placebo. Further, indirect evidence from randomized controlled trials (RCTs) and meta-analyses indicate that pre-endoscopic PPI may reduce need for endoscopic treatment and may benefit a minority of patients. However, ACG was specifically looking at mortality benefit and reduced risk of rebleeding, neither of which were consistently found among the various studies included in this guideline.
Pages: 1 2 3 | Single Page




No Responses to “ACEP Clinical Policies Committee reviews Gastroenterology Guideline Update”