This medical malpractice case covers a theme commonly seen in lawsuits against emergency physicians. It highlights the importance of carefully reviewing test results and communicating clearly with patients and other doctors.
Explore This Issue
ACEP Now: Vol 40 – No 03 – March 2021The Case
A 63-year-old man presented with a cough. His vital signs showed a heart rate of 123 bpm, blood pressure of 129/94, respiratory rate of 15/min., and oxygen saturation of 96 percent on ambient air. His past medical history was remarkable for chronic obstructive pulmonary disease (COPD) and a history of smoking. He was seen by a triage nurse, who noted chest congestion for one week as well as fever and chills.
The physician saw the patient and documented similar complaints. He also noted that the patient had body aches and “burning pain” with coughing. The review of systems noted the absence of fever and chills, conflicting with the triage documentation. The physical examination was relevant for diminished breath sounds, unlabored breathing, and the ability to carry on normal conversation.
A chest radiograph was ordered, and the patient was treated with DuoNeb (albuterol sulfate and ipratropium bromide). The chest radiograph interpretation is shown in Figure 1.
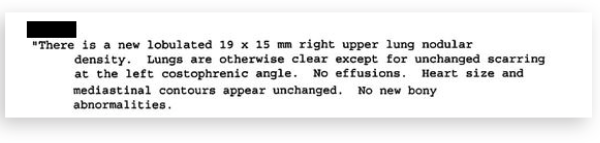
Figure 1: Chest Radiograph Interpretation
The physician documented an assessment of the cough, upper respiratory infection, and COPD. On reassessment, the patient was described as feeling “OK after visit.” The physician documented that the “chest X-ray shows some residual of COPD with no acute changes.”
The patient was advised to push fluids, use an inhaler, stop dairy, and follow up with his primary care physician (PCP) about the possibility of obtaining a nebulizer for home use.
The patient did not have any documented health care visits for the next three years.
Three years later, he presented to a new PCP to establish care due to the fact that he had been feeling short of breath and fatigued. Labs and a chest radiograph were ordered. The chest radiograph showed a significantly larger lung mass, and he was promptly referred for a CT scan and consultation with a pulmonologist. The CT scan results are shown in Figure 2.
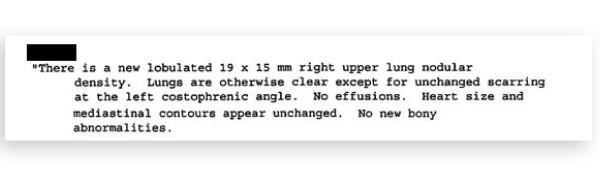
Figure 2: CT Scan Result
The patient was seen by pulmonology and ultimately had his case presented at the hospital’s tumor review board. He was deemed not to be a surgical candidate but underwent extensive chemotherapy and radiation treatment.
The medical record available in the court case ends with consultations from palliative care specialists. His medical outcome is uncertain, although a search of newspaper records did not turn up an obituary under the patient’s name.
Pages: 1 2 3 | Single Page





No Responses to “A Lack of Communication Let a Cancer Grow, Which Led to a Lawsuit”