The role of emergency physicians has been made dramatically more important due to the pandemic. The performance of EDs in 2020 and into 2021 changed abruptly, and that carried through into 2022. EDs weathered attacks from a variety of sources in recent years. Commercial payers aggressively abused the No Surprises Act as a method to delay, downcode, and deny payment for emergency services. ED leaders worked to develop new physician documentation and coding guidelines that needed to be implemented at the beginning of 2023. Software attacks crippled operations in large hospital chains, and physical assaults on ED staff continued unabated.
Explore This Issue
ACEP Now: Vol 42 – No 06 – June 2023The preliminary results of the 2022 Emergency Department Benchmarking Alliance performance measures survey found a significant deterioration in patient processing due to inpatient boarding. Preliminary results of the survey are being released to help emergency physicians understand that current challenges are occurring nationwide. These data can be shared with hospital administration as there is mutual need to find solutions to the current ED flow challenges and very high ED walkaway rates.
Patient volume losses in 2020 reversed in 2021. After drops of about 14 percent in overall ED volumes in 2020 compared to 2019, many EDs are managing patients at volumes near those of 2019 again.
A Lower Percentage of Children Present to EDs That Are Not Designated as Children’s Hospitals
In general community EDs, the decrease in visits by patients under age 18 bounced back from about 13 percent in 2021 to about 15 percent in 2022. The resurgence of respiratory syncytial virus and respiratory infections other than COVID-19 may explain this.
Patient arrival by EMS increased and more of those patients were admitted. About 20 percent of ED arrivals in 2022 came by ambulance, and 36 percent of those EMS patients were subsequently admitted, compared to about 14 percent of ambulatory arrivals.
ED patient throughput improved in 2022 in some regards, which is an incredible accomplishment in a very difficult year. Median “door to doctor” time remained steady at about 14 minutes. Long-term trends of improving ED patient intake remain intact, as times decreased in most years since 2008, when the intake time was about 41 minutes.
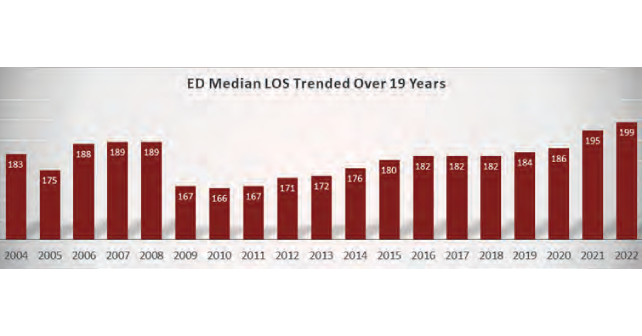
All ED patient-processing times increased remarkably in EDs, related to lengthy hospital boarding times. This necessarily increased ED walkaway rates. The overall length of stay for all ED patients increased to 199 minutes in 2022, up from 182 minutes in 2018 (see graph above).
Despite the work of many ED physicians and leaders to preserve flow, boarding times in 2022 jumped to 192 minutes, from 121 minutes in 2020. This time interval is very cohort-dependent, depending on ED volume. The time from “door to decision” was about 198 minutes in 2022, despite increased use of diagnostic testing.
The percentage of patients who leave the ED prior to the completion of treatment (LBTC) increased to 4.6 percent in 2022, compared to 2.7 percent in 2019. This is the highest LBTC rate that has ever been seen, and means that about 7 million patients who wanted ED care left without that service. That amounts to more than $1 billion dollars in lost ED physician revenue.
The Challenges to Emergency Physicians Are Significant
Reflecting on the management challenges of EDs in the upcoming years, there is need to improve hospital flow, safety, and quality. With the lessons and data of 2022 in mind, the need to move admitted patients up to inpatient units is an obvious management priority.
Executive Summary of ED Operations in 2022
Volume was up from 2021. Volumes collapsed in 2020, but in 2023 EDs are now nearly back to 2019 volumes.
Outstanding ED work through the pandemic saved patients, hospitals, and medical staffs.
There is an increasing percentage of patients arriving in EDs via EMS, now averaging about 19.7 percent. Admission rates for EMS patients is about 36 percent. Pediatric volume in community EDs is up.
Mental health cases and ED violence are up significantly.
Door-to-clinician median time is down to 14 minutes. But overall ED flow has deteriorated, with ED median length of stay for all patients 199 minutes in 2022.
Processing of ED patients to inpatient units is crippling ED operations. Boarding times crashed all types of EDs. The median boarding time across all EDs was about 192 minutes in 2022, up from 119 minutes in 2019.
Poor flow is an incredible stress on ED staff, resulting in loss of ED staff of all disciplines. Walkaways have more than doubled.
 Dr. Augustine is national director of prehospital strategy for US Acute Care Solutions based in Canton, Ohio; clinical professor of emergency medicine at Wright State University in Dayton, Ohio; and vice president of the Emergency Department Benchmarking Alliance.
Dr. Augustine is national director of prehospital strategy for US Acute Care Solutions based in Canton, Ohio; clinical professor of emergency medicine at Wright State University in Dayton, Ohio; and vice president of the Emergency Department Benchmarking Alliance.
Reference
- Managing and measuring emergency department care: results of the fourth emergency department benchmarking definitions summit. Maame Y, et al. Academic Emergency Medicine. 2020;27:600–611.
Pages: 1 2 3 | Multi-Page





One Response to “A First Look at Emergency Department Data for 2022”
June 15, 2023
Paul Mele MDSame problems we had 20 years ago
the solution costs money.
no one willing to spend it.