Lancaster General Hospital (LGH), in Lancaster, Pa., has long had a reputation for an efficient, busy, community hospital emergency department (ED). Now part of Penn Medicine Health System, it is a 525-bed, nonprofit, level I trauma center, and offers both Percutaneous Coronary Intervention (PCI) and stroke thrombectomy. It has American Nurses Credentialing Center magnet designation. Its ED sees 113,000 visits a year and a high volume of geriatric patients (28.5 percent). Prior to 2021, the ED boasted some of the best operational metrics reported in an ED of its size and could be considered a “best of breed.” Its door-to-doctor time was 25 minutes and its walkaway rate only 1.7 percent. After COVID-19, however, with increasing behavioral health (BH) volumes and increasing boarding, the department began to falter. In 2021 those metrics were 40 minutes and 9.2 percent, respectively.
Explore This Issue
ACEP Now: Vol 42 – No 05 – May 2023While the community presented with as many BH complaints as chest pain chief complaints, there was no comprehensive service line dedicated to mental health issues. In addition, the community resources for such patients were limited. Historically, the ED had operated under a traditional flow model, beginning with nurse triage, and with further health care interactions operating in series in the main department. They had not begun a flow model involving a physician in triage (PIT), which is now considered a best practice for high-volume EDs.
Thinking Differently
LGH decided that their current structure was not functioning and that a new flow model was required, particularly for the BH patients. Because they had a vast waiting room with more than 70 plexiglass-enclosed chairs, but treatment spaces with beds were limited in the main part of the ED, LGH began thinking about ways to use existing resources differently.
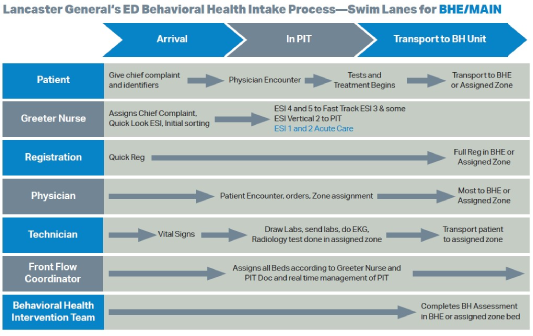
A task force set out to manage BH patients differently. The ED clinical team—in conjunction with the dedicated BH team—worked collaboratively together to determine best flow for patients arriving with a BH complaint. When the PIT doc is present, patients are seen and assessed in tandem by a triage nurse and a physician. The PIT team can initiate a BH consult while the patient remains in triage; when possible, patients are discharged directly from the triage area after the medical screening exam and the BH team assessment (backed by a psychiatrist). This has resulted in a reduction in one-to-one sitter usage for discharged patients, and expedites bed search for patients requiring psychiatric admission.
Pages: 1 2 | Single Page





No Responses to “A Behavioral Health Intake-Process Model”