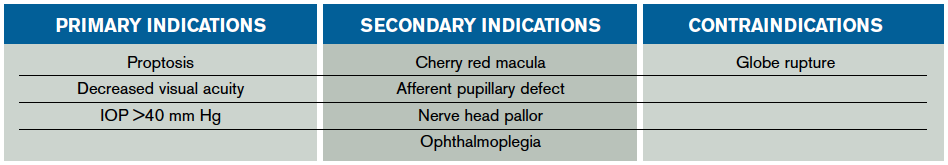
The indication to perform a lateral canthotomy does not change regardless of the underlying cause. Astute emergency physicians will attempt to uncover the cause of OCS in the setting of multiple etiologies not commonly mentioned in texts or the literature. The commonly cited retrobulbar hematoma is only one of many underlying etiologies requiring emergent decompression. Others include orbital cellulitis; foreign material; orbital edema (trauma, massive fluid resuscitation, thermal injuries); orbital emphysema; intraocular injections; postoperative complications from periorbital surgery; caustic injuries; or retrobulbar hemorrhage from thrombolysis, sickle cell disease, or leukemia.1 In the setting of any of the aforementioned injuries or disease processes, physicians should look for primary or secondary indications to perform a lateral canthotomy to preserve vision. Primary indications include proptosis and decreased visual acuity or IOP >40 mm Hg, while secondary indications are more subjective findings such as an afferent pupillary defect (APD), ophthalmoplegia, nerve head pallor, or a cherry red macula (see Table 1).3
Explore This Issue
ACEP Now: Vol 34 – No 03 – March 2015
Physicians should look for any sign of orbital compartment syndrome and immediately move forward with a lateral canthotomy once the decision is made because “time is vision.”
A Paper Clip and a Morgan Lens: Tricks for Lateral Canthotomy
Performing a lateral canthotomy is a heroic—yet stressful—potentially vision-sparing procedure all emergency physicians prepare for and yet rarely perform. When the time comes to perform a lateral canthotomy, emergency physicians may play back Roberts & Hedges’ Clinical Procedures in Emergency Medicine in their mind to carry out each step. It seems so simple, almost mindless, to cut the lateral canthal tendon—that is, until you add in the periorbital edema and chemosis that impairs visualization for the procedure. While there are several strategies to help improve visualization, and therefore success rates, using a paper clip bent into a hook to displace the eyelid for the procedure is a safe adjunct and utilizes equipment easily found in any ED.
Any time emergency physicians perform a procedure such as a lateral canthotomy, providers experience a surge of endogenous catecholamines leading to tachycardia, perspiration, and even tremors. With one slip of the hand, the iris scissor point can accidentally penetrate the lateral aspect of the globe, leading to an iatrogenic globe rupture. What if this fear could simply be put to rest by a device readily found in all EDs? A Morgan lens can be placed on the cornea prior to the procedure to act as a shield to prevent iatrogenic globe rupture.
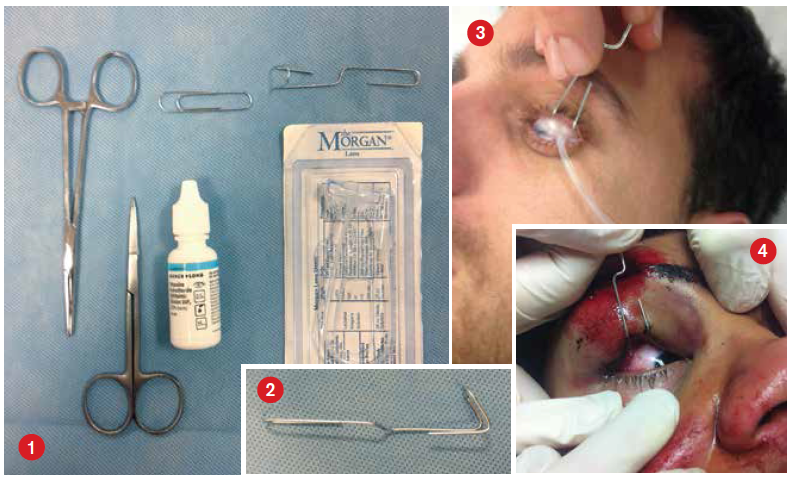
Equipment (see Figure 1)
- One Morgan lens
- Medium-sized paper clip
- Topical anesthetic ophthalmic drops (eg, tetracaine)
- Standard equipment for lateral canthotomy and cantholysis
Technique
- Place the patient in a comfortable supine position at a height suitable for you to perform the lateral canthotomy and cantholysis.
- Bend the medium-sized paper clip into a hook with a handle (see Figure 2) that can be used to retract the eyelids for the procedure (see Figure 3). (Paper clips can be used for both upper and lower eyelids if deemed necessary for visualization.)
- Place two drops of topical anesthetic ophthalmic drops into the eye in which you will be performing the lateral canthotomy. (Caution: Do not use the anesthetic drops prior to checking the pH if the underlying etiology is a caustic exposure.)
- Place the Morgan lens into the affected eye prior to the start of the lateral canthotomy and cantholysis (see Figure 3). No irrigation fluid is necessary.
- Have an assistant use the paper clip to hook the eyelid and retract it to improve exposure and visualization during the procedure (see Figure 4).
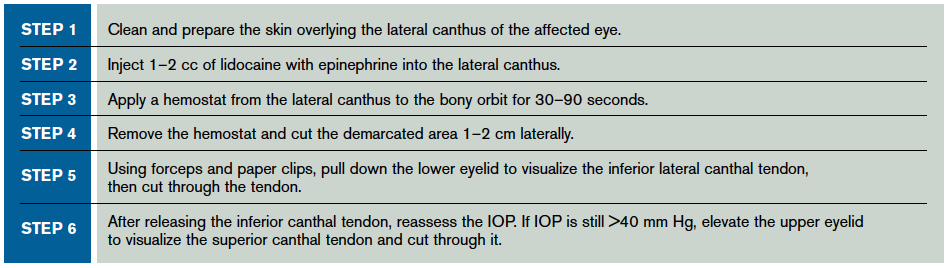
- Perform the lateral canthotomy and cantholysis (see Table 2).
Pages: 1 2 3 4 | Single Page





2 Responses to “Tips for Relieving Increased Intraocular Pressure”
April 5, 2015
John Patrick MDA more accurate title for this would be “Tips for Relieving Increased Intraorbital Pressure” or “Tips for Relieving Secondarily Increased Intraocular Pressure”
April 9, 2015
neat trick: morgan lens for lateral canthotomy | DAILYEM[…] References: ACEP Now article + picture from article […]