
Explore This Issue
ACEP Now: Vol 40 – No 06 – June 2021Figure 4A: Poorly visualized needle due to low angle of insonation.
Figure 4B: Improved needle visualization after “toeing in” transducer.
Optimizing Needle Visualization by Hydrolocation and Hydrodissection
Hydrolocation and hydrodissection are additional techniques that help localize the needle tip during an in-plane ultrasound-guided nerve block.
Hydrolocation refers to a gentle yet rapid deposition of a small amount of normal saline to produce a small anechoic window, allowing better needle tip visualization. Hydrodissection uses this same fluid to dissect structures, classically fascial planes, when performing nerve blocks, providing confirmation of the proper location and fluid anesthetic placement.

Figure 5A: Standard transducer positioning.
Figure 5B: Operator “toes in” transducer.
During hydrolocation, as the clinician approaches the ideal location for anesthetic deposition, small aliquots of normal saline (<0.5–1 mLs) are gently pushed (with the help of an assistant) to visualize the needle tip. If the sonographer is off-axis (ie, the transducer is not in-plane with the needle shaft and tip), the sonographer will not see anechoic fluid coming from the needle tip. The sonographer can adjust the needle or transducer, and the assistant can inject another small aliquot to confirm needle tip localization.
During hydrodissection, we recommend using the overlying fascial plane as an optimal landmark for needle tip placement and anesthetic deposition. Using aliquots of normal saline (2–5 mL), the goal is to clearly visualize the opening (expansion) of targeted fascial planes with anechoic fluid (see Figure 6). Only then should an assistant gently infuse the anesthetic. If the clinician does not produce a clear anechoic pocket separating the targeted fascial planes, they are not in the desired space. Once the fascial plane is clearly opened with anechoic normal saline, we recommend slowly and gently depositing anesthetic for optimal block success.2
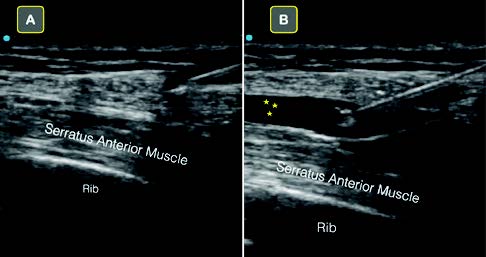
Figure 6A: The clearly visualized needle tip is seen above the serratus anterior muscle.
Figure 6B: Note that normal saline is used to hydrodissect the fascial plane that lies just above the serratus anterior muscle. Once this anechoic space is clearly defined, anesthetic can be safely deposited.
Conclusion
Ultrasound-guided nerve blocks are becoming an important clinical skill for emergency physicians. They provide directed anesthetic deposition, reduce reliance on opioids, and can even replace procedural sedation in some cases.
In our experience teaching ultrasound-guided nerve blocks, locating the needle tip during in-plane blocks is often the most challenging aspect of a procedure. Optimizing ultrasound screen positioning, properly stabilizing the ultrasound transducer with the nondominant hand, “toeing in” the transducer for steep blocks, and using normal saline to both hydrolocate the needle tip as well as hydrodissect fascial planes improve success.
We hope these easily incorporated block “microskills” will improve your confidence when performing your next ultrasound-guided nerve block.
Pages: 1 2 3 4 | Single Page





No Responses to “Tips for Performing Ultrasound-Guided Nerve Blocks in the Emergency Department”